
Electrolytes and Minerals
last authored:
last reviewed:
Introduction
Potassium and magnesium are the major cations inside cells, while sodium is the major extracellular cation. Phosphate and protein are the major intracellular anions, with chloride and bicarbonate outside.
- bicarbonate
- calcium
- chloride
- iron
- iodine
- magnesium
- phosphate
- potassium
- sodium
- zinc
Bicarbonate
Sources
Needs
Absorption
Regulation
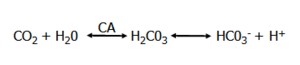
The physiologic concentration of HCO3 is 24 mmol/l, while the concentration of H+ is 40 nmol/l.
Bicarbonate Reabsorption in the Kidney
The kidney has the capacity to regulate blood pH by addition or secretion of bicarbonate.
Normally, all HCO3 is reabsorbed, giving urine a pH of less than 7. Vegans have a more alkaline diet, and so some HCO3 is excreted in the urine. Addition of large amounts of HCO3- to the blood will be dealt with rapidly by the kidney through excretion.
Loss of bicarbonate produces renal tubular acidosis.
Seventy percent of HCO3 reabsorption occurs in the proximal tubule, with the rest in the LoH.
In the proximal tubule,
- HCO3 reabsorption is coupled with H+ secretion the Na/H antiporter.
- CA works both in the lumenal brush border and inside the cell.
- HCO3 reabsorption is coupled with NH4 secretion, mediated by deamination of glutamine from the liver.
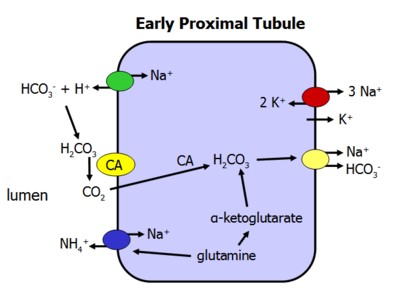
Transport defects, or inhibition of any of the above pumps, can result in renal tubular acidosis.
The drug acetazolamide inhibits CA and therefore reduces bicarbonate reabsorption.
After filtration, almost all bicarbonate is reabsorbed by the proximal tubule.
Functions in the Body
Deficiency
Toxicity
Calcium
Calcium is the most prevalent divalent cation in the body, occurring mainly in the bone but also playing key roles in the function of nerve and muscle cells.
Sources
Bioavailability is important for calcium absorption. Foods rich in calcium include:
- dairy products and fortified soy/orange juice
- dark, green, leafy vegetables
Supposedly, calcium carbonate is better absorbed if taken with acidic meals, and you can only absorb 500 mg of elemental calcium at one time.
Needs
An adult has about 1000 g of calcium in the body - 99% of it in bones and the rest in the extracellular fluid and soft tissue.
Although there is some controversy surrounding the lower limits of what is required, estimates include:
- 4-8 : 800 mg
- 9-18: 1,300 mg
- 19-50: 1,000 mg
- > 50: 1,500 mg
- pregnant or lactating: 1,000 mg
Plasma Levels
Normal blood calcium levels are 8.0-10.4 mg/dl, or 2.00-2.60 mmol/L, while normal intracellular calcium levels are 10-4 mmol/L (check this).
In the plasma, 45% is protein bound, 5% is complexed to other ions such as citrate and phosphate, and 50% is free ionized Ca2+.
Plasma calcium and phosphate concentrations are close to the saturation point at which calcium phosphate precipitates out of solution onto the bone matrix. Accordingly, plasma values of the two ions are inversely related, as a rise in one will cause a fall in the other.
Serum calcium levels depend on albumin, requiring a correction of increased sCa2+ by 0.2 mmol/L for a decrease in 10 g/L (below 40 g/L) of albumin.
For example, a sCa2+ of 1.9 mmol/L and albumin of 20 g/L requires an increase in sCa2+ of 0.4 mmol/L, resulting in a corrected value of 2.30 mmol/L.
Another formula states (Albnor - Albpt)0.8 + Ca2+pt
Ionized calcium levels are 4.25-5.25 mg/dl, or 1.05-1.30 mmol/L. This is an important indicator of clotting capacity.
Absorption
Of dietary calcium, 25-30% is absorbed in the gut, mainly in the duodenum and proximal jejunum. Absorption occurs transcellularly and is increased by the hormonal action of 1,25(OH2)D3, the active form of vitamin D.
Regulation
It is critical to maintain levels of ionized calcium in the extracellular fluid in maintain function of nerves and muscle.
The parathyroid gland monitors levels of ionized calcium in the plasma. PTH and vitamin D increases calcium levels, while calcitonin decreases them.
Following filtration in the kidney, 70% is reabsorbed in the proximal tubule and a further 20% in the thick ascending loop of Henle. The latter is controlled by the voltage differential generated by active Na/Cl/K absorption and is mediated by the Ca2+-selective paracellular pathway.
As calcium reabsorption depends on sodium movement in the loop of Henle, diuretics such as furosemide can lead to hypocalcemia. In contrast, thiazides can actually enhance calcium reabsorption.
Hormonal control
Calcium transport in the distal tubule , accounting for 5-10%, is active, transcellular, and the major target for hormonal control by PTH and vitamin D. In order to keep intracellular levels low, calcium-binding proteins are used. Lumenal uptake proceeds down an electrochemical gradient through Ca2+ channels regulated by PTH, while Ca2+ export is active and depends on the Na+/Ca2+ exchanger or a Ca2+ ATPase. Both Ca2+-binding proteins and Ca2+ ATPase are under control of vitamin D.
Functions in the Body
Most of the calcium in the body is present in the bone, where it combines with phosphate to form hydroxyapetite, the building block of bones.
Calcium is a key mediator of muscle cell (myocyte) contraction. Calcium enters the cytoplasm from outside, and from the sarcoplasmic reticulum of these cells, doing something with myosin and leading to contraction.
Calcium plays an even more important role in cardiomyocytes.
Calcium is invloved in neutrotransmitter release.
Along with the functions in the specialized cells already listed, calcium is also a key component of signaling patwhays in all cells. Intracellular levels are kept very low, with most calcium bound to proteins or sequestered in the endoplasmic reticulum or mitochondria.
DAG, PI3K, ER, etc
Calcium also plays a role in coagulation. Citrate acts by binding calcium, preventing clotting.
Deficiency
Please see hypocalcemia.
Toxicity
Please see hypercalcemia.
Chloride
Sources
Needs
Absorption
Regulation
After filtration through the glomerulus, almost all chloride is reabsorbed by the nephron. At least 60% is reabsorbed by the proximal tubule.
Functions in the Body
Deficiency
Toxicity
Iron
Organic, is iron bound to heme. Inorganic refers to free iron.
Ferrous (Fe 2+) is soluble, while ferric (Fe 3+) is insoluble.
Sources
Dietary iron is the primary source of iron. Meats have much more bioavailable iron than vegetables, which also contain absorption-inhibiting phosphates and phytates. Sources include:
- meat, fish, poultry, organ meats
- eggs
- prunes and raisins
- peas, beans, lentils
- soy
An adult male takes in 15-20 mg/day, while females take in 10-15 mg daily.
Red blood cell turnover releases 25-30 mg of iron each day into the marrow and spleen, with transport back to sites of new red blood cell production.
Normal men have a total body iron content close to 4000 mg, with 500-1000 mg in storage. Women usually have less than 200 mg iron storage levels.
Needs
Iron measures of the blood can be use to estimate total iron.
Pregnancy increases iron requirments by 1g elemental iron per fetus. This is broken down into 500mg for fetal and placental growth, 500mg for increased maternal RBCs, and 200mg for losses. Most iron is transferred after 26 weeks.
All pregnant women should receive 150mg ferrous sulfate, 300 ferrous gluconate, or 30mg ferrous iron daily during secind and 3rd trimester. If anemic, pregnant mothers should take 1 g ferrous sulfate, or 180mg elemental iron.
Premature infants have lower stores of iron and increased external losses. Their rapid growth necessitates greater need - perhaps 2 mg/kg/day
Term infants have total iron supplies of 75 mg/kg, making iron deficiency rare before 4 months
Infants 4-12 months have a very large iron need as their birth weight doubles by 5 months and triples by 12 months. They need 1 mg/kg/day.
Children 1-4 years have the highest prevalence of iron deficiency, often due to "milk baby syndrome", where babies drink loads of milk and little else. Toddlers need 10 mg/day.
School-aged children rarely have iron deficiency due to nutritional status, making detailed investigations necessary.
Adolescents are increased risk of iron deficiency due to increased growth, the onset of menstration in girls, and often poor diets.
Men need x, but they normally ingest 15-20 mg of iron daily.
Women need x, but they normally take in 10-15 mg iron daily.
Absorption
Iron is most absorbed in the proximal small intestine.
Organic (heme) iron binds to mucosal cell receptors and passes into the cytoplasm, where the porphyrin ring is cleaved and the iron released.
Inorganic iron is converted to ferrous iron and bound to transferrin. Its absorption is increased by the presence of heme iron and decreased by the presence of phytates and phosphates.
Intracellular iron is transported to the liver via the portal circulation for metabolism. The plasma protein transferrin is reponsible for this. At any one time, about 3 mg of iron is found in the blood.
Transferrin secretion by the liver is inversely proportional to hepatic iron stores.
Excess iron in the gut combines with apoferritin on mucosal cells, where it is bound and lost through sloughing off. Levels of apoferritin are proportional to levels of iron stores.
Regulation
Functions in the Body
Iron's key role is as a component of heme, the component of hemoglobin which binds oxygen for transport around the body. It is distributed across the body in the following locales:
- hemoglobin - 65%
- ferritin and hemosiderin - 22%
- myoglobin - 10%
- enzymes - 3%
co-factor for some neurotransmitters.
Deficiency
Iron deficiency is most serious for causing anemia, which is usually microcytic (small red blood cells). See iron deficiency anemia for more details.
Toxicity
Iron toxicity can cause nutritional hemosiderinosis and organ damage. It is a direct GI irritant. It is the amount of elemental iron that determines toxicity. Intracellular iron is the worst offender.
Iron can enter the blood and cause an anion gap.
gastrointestinal
cardiovascular
|
neurological
other
|
Five stages of toxicity, but in practice
- stage 1: abdominal pain, diarrhea, vomiting; absence of these in 1st 6 hours effectivey excludes diagnosis
- stage 2: 6-24 hours: not always seen. GI symptoms improve
- stage 3: systemic toxicity: coagulopathy hepatica, renal, cardiac
- stage 4: hepatic stage 2-5 days
- stage 5: delayed 4-6 weeks: gastric obstruction
Copper
Sources
Needs
Absorption
Regulation
Functions in the Body
Iodine's principal use is in the thyroid gland, where it is an integral part of T4 (thyroxine) production.
Deficiency
Iodine deficiency results in hypothyroidism due to a lack of T4 production. This results in a a loss of normal inhibitory feedback, such that large levels of TRH and TSH are secreted.
High TSH levels stimulate the thyroid gland to grow enormously in an attempt to make more T4, which it cannot do. This growth is called goiter.
Iodine deficiency is incommon in developed countries due to its presence in table salt. However, it is still a public health problem in areas such as Africa and China, where rainwater has leached iodine from the soil.
Toxicity
Magnesium
Of the body's magnesium, 54% is in the bone, 45% in the soft tissues and 1% in extracellular fluid.
Sources
- meat
- dairy products
- soy
- clams and other seafoods
- whole grains and wheat germ
- almonds and other nuts
Needs
Intake increases with growth, pregnancy, and lactation.
Absorption
All Mg2+ that is not protein-bound is filtered through the kidney's glomerulus. Following filtration, 30% is reabsorbed in the proximal tubule. Another 65% is paracellularly reabsorbed in the thick ascending loop of Henle, controlled by the voltage differential generated by active Na/Cl/K absorption. A further 5% is reabsorbed in the distal tubules. Magnesium handling is directly influenced by sensors which measure plasma magnesium ions.
PTH and calcitonin increase paracellular reabsorption, possibly by influencing tight junction permeability.
Booth loop diuretics and thiazides increase magnesium excretion.
Regulation
Functions in the Body
Magnesium is critical in the function of over 300 intracellular enzymes, for the phosphorylation of ATP, for smooth muscle contraction, and neurological membrane potentials.
Deficiency
Magnesium deficiency can cause:
- weakness
- convulsions
- neuromuscular irritability
- failure to thrive
Toxicity
Signs of magnesium toxicity include:
- depressed deep tendon reflexes
- decreased respiratory rate, respiratory failure
- anuria
- hypotonia
- hypotension
- cardiac disturbances
Calcium IV is the antidote.
Phosphate
An adult has about 600 g of phosphate. 85% is skeletal, with the rest in the ECF and tissues. Only 0.1% of the body's phosphorus is in the plasma.
About 65% of phosphate is absorbed, mainly in the duodenum and jejeunum transcellularly in a process enhanced by vitamin D.
Of plasma phosphate, 55% exists as free phosphate in the form of HPO42- and H2PO4- , which act as a buffer pair.
Sources
Needs
Absorption
Regulation
Plasma calcium and phosphate concentrations are close to the saturation point at which calcium phosphate precipitates out of solution onto the bone matrix. Accordingly, plasma values of the two ions are inversely related, as a rise in one will cause a fall in the other.
Renal phosphate regulation
All phosphate not protein-bound is freely filtered through the glomerulus.
The maximum rate of reabsorption along the nephron is limited, and everything above a threshold is excreted.
Of that filtered, 80% is reabsorbed in the proximal tubules in a transcellular process relying on sodium reabsorption. Apical phosphate entry is controlled by PTH.
There is no significant phosphate transport in the loop of Henle. Distal tubules reabsorb a further 10% and the collecting ducts 2-3% in a manner appearing similar to that of the proximal tubules.
Functions in the Body
Of plasma phosphate, 10% is protein bound, 35% is complexed with ions such as sodium, magnesium, and calcium, and 55% is ionized.
Phosphate is a key component of cell membranes.It is also used to produce ATP and is an essential component of DNA and RNA.
Deficiency
Toxicity
Potassium
Potassium is the major intracellular cation, playing a critical role in the membrane potential of excitable cells. The body contains about 3500 mEq of potassium.
Intracellular [K+] is about 150 mM, while normal plasma [K+] ranges from 3.5-5 mM/L. Accordingly, only 2% of total body potassium is outside cells.
Plasma [K] is a poor indicator of total body stores.
Sources
Bananas are the best known source of potassium. Others include:
One choice= 3 mmol
- tomatoes
- cantelope
- honeydew
- peaches
- meat
- milk
- potatoes
- dried beans
- squash
- prunes and raisins
- oranges and grapefruits
Between 40-120 mmol of K+ is taken up through the gut daily.
Needs
Absorption
Regulation
Cellular Homeostasis
In response to dietary potassium, rapid removal from the extracellular space is necessary to prevent life-threatening hyperkalemia.
Potassium can easily move across membranes, and there are several mechanisms that regulate its transport:
Increases K+ Entry |
Decreases K+ Entry |
|---|---|
|
|
Renal filtration and secretion
Average daily intake is 40-120 mmol. As plasma levels are 3.5-5 mmol, and the kidneys filter 180L daily, alomst 800 mmol of K+ is filtered. To maintain its balance, the kidney only excretes 5-15% of filtered K+.
Potassium, similar to other electrolytes, is freely filtered through the glomerulus. Almost all potassium is reabsorbed by the time filtrate reaches the collecting tubules. Potassium destined to be excreted is secreted into the collecting duct.
All cell types have potassium channels, which vary according to cell type. Each is a tetramer. Tubular cells habe different pumps and channels on their apical and basolateral aspects. The major driving force is the Na/K ATPase.
The ROMK channel is present along the kidney, save the proximal tubule. They tend to be open and allow potassium to flow out of the cell, allowing for secretion in the principal cells of the cortical collecting ducts.
Site |
Mechanism |
% |
Inhibitor |
Stimulator |
|---|---|---|---|---|
proximal |
unknown channels; may follow Na and water paracellularly
|
65 |
|
|
thick ascending loop |
Na/K/Cl2 triporter significant paracellular movement driven by +ve potential |
30 |
||
distal |
sodium-dependent |
5 |
|
|
collecting duct |
principal cell secretion |
variable |
|
|
90% eliminated through the kidney and 10% in the stool.
The Na/K ATPase drives potassium secretion in principal cells by pumping basolaterally, allowing apical secretion through K+ channels or chloride co-transporters. Sodium reabsorption results in negative lumenal potential, promoting potassium secretion.
Potassium secretion into the lumen will only continue if filtrate concentration is kept low. Accordingly, the higher the flow rate, the higher the level of K+ secretion down its concentration gradient into the lumen.
Excretion is also increased by:
- aldosterone
- sodium delivery to the collecting duct (eg, diuretics)
- high serum potassium level
- delivery of negatively charged ions to the collecting duct (eg, bicarbonate)
- increased intralumenal acidity
Excretion is decreased by
- absence or relative deficiency of aldosterone
- low sodium delivery to the collecting duct
- low urine flow
- low serum potassium level
- renal failure
Functions in the Body
Potassium is a key excitatory signal.
The K+ gradient - ratio of intracellular to excellular potassium - ie is the major determinant of cell membrane resting potential.
Potassium enters cells using a pump-leak mechanism, whereby they are pumped in through the Na/K ATPase and leak out through various channels. Potassium concentration can be controlled by changing pump activity, pump number, or channel permeability.
Nervous System
Cardiovascular System
Potassium is responsible for repolarizing cardiac pacemaker and muscle cells. Following influx of sodium and calcium during depolarizing, potassium flow down its concentration gradient and out of the cell restores intracellular negativity.
Deficiency
see hypokalemia
Toxicity
see hyperkalemia
Sodium
Sodium is the major extracellular cation, and its concentration is tightly to ensure physiologic functioning.
Normal sodium concentrations
Normal plasma sodium concentration is 137-145 mmol/L.
Sources
Needs
While guidelines recommend less than 2.5 g of sodium daily, average intake in the West ranges from 2-10g (check this).
Amounts of water in the body is directly propotional to sodium levels, and weight gain or loss accompanies changes in sodium intake to maintain homeostatic concentrations. Abrupt changes in sodium intake will create a period of positive or negative sodium balance as the kidney takes 12-24 h to adjust levels of sodium excretion to match intake.
Absorption
Sodium absorption largely occurs in the colon, where it passes through aldosterone-regulated channels. Sodium's concentration gradient is used for the absorption of monosaccharides and amino acids via co-transporters in the gut, primarily in the jejeunum. Each of these mechanisms is dependent on Na/K ATPase function.
Sodium can also be absorbed paracellularly, and as is the case for water, this is most effective in the duodenum due to its 'looser' tight junctions.
Regulation
Sodium is freely filtered in the kidney glomerulus, leaving filtrate concentration similar to that of blood. The 180 L of blood filtered daily through the kidney contain almost 2kg (25.5 Mol) of sodium, and with 2-10g taken in daily, the vast majority of it (25.4 Mol) must be reabsorbed. About 5% of salt intake is lost through sweat or through feces.
A huge amount of this occurs in the proximal tubule and loop of Henle, and the remaining amount is under precise regulation in the distal tubules and collecting ducts to maintain salt balance.
Sodium leaves the tubule lumen via electromotive and osmotic forces along its gradient, but is pumped out against its gradient into the interstitium via the Na/K ATPase. It then passes freely into the blood to complete reabsorption. The kidney uses 7-10% of the body's oxygen demands, even though they account for less than 0.5% of total body weight. This is in parge part due to activity of the Na/K ATPase and its role in Na+ reabsorption.
Site |
Mechanism |
% |
Inhibitor |
Stimulator |
|---|---|---|---|---|
proximal |
Na/H exchanger, Na-X symporter |
65 |
||
thick ascending loop |
Na/K/Cl2 triporter |
25 |
||
distal |
Na/Cl symporter |
5 |
||
collecting duct |
ENaC channels in principal cells |
2-5 |
In the proximal tubule, the sodium gradient drives co-transport of bicarbonate, amino acids, glucose, and other organic molecules.
Regulation of GFR increases or decreases the amount of sodium passing through the tubules. NaCl concentration is sensed in the macula densa of the kidney, with low levels of NaCl causing renin release.
Increased plasma osmolarity signals increased thirst and ADH secretion in order to increase plasma volume. Interestingly, it also increases salt appetite.
Increased sodium absorption
ADH is primarily involved with reguation of water retention. It also increases sodium channels in the TAL, increasing plasma osmolarity in order to draw water in. Volume takes precedent over free water.
Increased flow leads to elevated GFR. An increased filtration fraction decreases hydrostatic pressure in the peritubular capillaries, increasing the driving force from the interstitium to the capillaries and thereby increasing absorption of fluid and NaCl.
Sympathetic innervation has three major functions:
- markedly reduces blood flow and GFR, slowing Na excretion
- increases renin secretion
- enhances sodium reabsorption through activation of the Na+/H+ exchanger
Ang II, activated by renin secretion:
- increases aldosterone secretion
- lowers the setpoint of the tubuloglomerular feedback mechanism
- enhances the Na/H exchanger in the proximal tubule and thick ascending limb to increase sodium reabsorption
Aldosterone increases Na channels, Na/K pumps, and ATP production in the principal cells of the distal tubule and collecting duct, increasing Na resorption. Aldoserone's effects primarily occur in the kidney, but it also works on sweat glands and the colon to increase sodium reabsorption.
Increased Sodium Excretion
ANP binds to prinicpal cells and activates guanylyl cyclase, which produces cGMP that inhibits ENaC channels. ANP also inhibits aldosterone release and renin production, increasing GFR by dilating afferent arterioles. The net effect is to increase sodium excretion.
Prostaglandins and Bradykinin are produced locally in the kidney and inhibit sodium reabsorption.
Dopamine is produced in the kidney from circulating L-dopa and causes renal vasodilation, leading to increased Na excretion. It also directly inhibits Na reabsorption.
Collecting duct
Sodium is reabsorbed via the epithelial Na+ channel (ENaC) at the lumen and transported basolaterally by the Na/K ATPase. The hormones aldosterone and ADH both increase Na+ resorption, while prostaglandins, ANP, and nitric oxide reduce it.
Functions in the Body
Deficiency
see hyponatremia
Toxicity
see hypernatremia
Zinc
Sources
Needs
Absorption
Regulation
Functions in the Body
Deficiency
Toxicity
Movement of specific ions is the basis of the action potential. It depends on two major factors:
energetic favorability
concentration gradients and transmembrane potentials (voltage) are important factors in attracting or repelling given ions. For example, the low concentration of sodium inside the cell, as well as a negative resting potential, combine to drive sodium entry into cells.
membrane permeability
ion channels are important means of ion entry. but there is a lot more to the story than this. There is a great book - Cells, Gels, and the Engines of Life - which is worth a read for those interested in ion flux across membranes.
Flux of Other Electrolytes in the GI Tract
Sodium and chloride is absorbed in the colon, potassium is secreted. While Bicarbonate appears to be absorbed also, it is being broken down into water and carbon dioxide.
Diarrhea whille therefore cause a loss of bicarbonate, resulting in metabolic acidosis, and posassium, causing cardiac arrhythmias.
luminal conc. (mM) |
Na |
K |
Cl |
HC03 |
|---|---|---|---|---|
small intestine |
140 |
8 |
60 |
70 |
large intestine |
40 |
90 |
15 |
30 |
There is little evidence of any benefit of multivitamin use on cancer and cardiovascular disease (Fortmann et al, 2013).
Resources and References
Fortmann S et al. 2013. Vitamin and Mineral Supplements in the Primary Prevention of Cardiovascular Disease and Cancer: An Updated Systematic Evidence Review for the U.S. Preventive Services Task Force. Ann Intern Med. 159(12):824-834-834.
