
Hemoglobin
last authored:
last reviewed:
Introduction
Hemoglobin is found in red blood cells and belongs to the family of hemeproteins, which contain heme as a prosthetic group. In hemoglobin, as well as myoglobin, the heme group serves to reversibly bind oxygen during its transport around the body.
Heme is a complex of protoporphyrin IX and iron (Fe2+), with the iron bound to four N atoms in the porphyrin ring.
Hemoglobin is a tetramer of two pairs of globin polypeptide chains, with each subunit predominantly alpha helical and containing a heme group. Adult hemoglobin can be thought of as two identical αβ dimers. The alpha and beta chains are held tightly together, while dimers can move in relation to each other.
The gene for alpha globin, on chromosome 16, is duplicated, resulting in 4 copies per diploid cell. The gene for beta globin is on chromosome 11, giving it the normal 2 copies per diploid cell.
Due to its tetrameric state, each hemoglobin molecule can transport four oxygen or carbon dioxide molecules.
Different hemoglobins are comised of different subunits. While HbA is the major adult form of Hb, others are also present.
Form |
Chain |
Fraction of Total Adult Hb |
|---|---|---|
HbA |
α2β2 |
90% |
HbA2 |
α2δ2 |
2-5% |
HbA1C |
α2β2-glucose |
3-9% |
HbF |
α2γ2 |
<2% |
Gower 1 |
ζ2ε2 |
embryonic |
Gower 2 |
α2ε2 |
embryonic |
HbF |
ζ2γ2 |
embryonic |
HbF, or fetal Hb, has a higher affinity for oxygen than HbA, allowing oxygen transfer across the placenta. HbF levels decrease quickly to very low levels within 6 months of birth.
HbA2 is a minor component of adult Hb.
HbA1C represents the slow, non-enzymatic glycosylation of HbA, and depends on circulating glucose levels. As RBCs live for ~120 days, testing levels of HbA1C shows long term blood glucose levels.
Hemoglobin Synthesis
As erythropoietin triggers stimulation of red blood cell progenitors, there is a coordinated induction of heme and globin synthesis, with an increase in tranferrin receptor expression, required for iron transport.
Hemoglobin synthesis requires adequate supply of iron and normal production of protoporphyrin and globin. Iron is stored as ferritin, while excess porphyrin is complexed to zinc.
Rate of hemoglobin synthesis is determined by the availability of transferrin iron and levels of intracellular heme. Hemoglobin synthesis is highest in mature marrow erythroblasts and to a lesser degree in marrow reticulocytes.
Oxygen Binding Capacity
Deoxyhemoglobin is called the taut (T) form, and has a low oxygen affinity. Hemoglobin that has bound oxygen is called the relaxed (R) form, and has a high oxygen affinity.
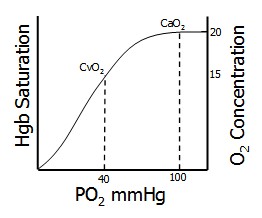
As the four potential oxygens become bound to hemoglobin, oxygen affinity goes up, forming a sigmoid-shaped curve. The first oxygen has difficulty binding, but after this the others bind easily. The last oxygen binds 300 times more effectively than the first. This is termed cooperative binding, and occurs through heme-heme interactions. Cooperative binding allows hemoglobin to lead and unload oxygen following small changes in the partial pressure of oxygen, as occurs between the tissues and the lungs.
Allosteric Effects
In general, factors that decrease oxygen affinity represent situations of low oxygen and facilitate oxygen delivery to tissues.
The Bohr Effect facilitates oxygen release from Hb when the pH is decreased, or when pCO2 is increased, by lowering oxygen affinity. Conversely, increases in pH or lowered pCO2 increased oxygen affinity. pH can drop following lactic acid buildup and causes increased oxygen release in the tissues. The Bohr Effect occurs because the deoxy form of Hb has a greater affinity for protons, resulting in the formation of salt bridges and a stabilized deoxy form.
2,3-BPG, or 2,3-bisphosphoglycerate, is an organic phosphate intermediate of glycolysis found in RBCs. 2,3-BPG binds to deoxy-Hb but not oxy-Hb, decreasing oxygen affinity. 2,3-BPG levels increase under chronic hypoxia, facilitating oxygen release in tissues. Transfused blood is often stripped of 2,3-BPG, resulting in an oxygen trap that can be serious. Substrates such as inosine that can enter the glycolytic pathway and be converted into 2,3-BPG are often used in transfused blood.
Carbon dioxide is usually transported as bicarbonate, but some is bound to Hb as carbamate (COO-). This stabilizes the T form of Hb (deoxy-Hb) and decreases oxygen affinity.
Carbon monoxide binds tightly to the Hb iron, shifting Hb to the R form and increasing oxygen affinity. This shifts the curve to the left and forms a parabola, hindering oxygen release. CO has over 200x the affinity for Hb than oxygen, meaning even small amounts of CO can be toxic. CO poisoning is treated with 100% oxygen, facilitating CO dissociation from Hb.
Myoglobin
Myoglobin, another hemeprotein, is found in cardiac and skeletal muscle cells, functions as an oxygen reservoir. Myoglobin binds oxygen more tightly than hemoglobin. Myoglobin's, eight alpha helices enclose the heme group.
