
Fever
last authored: March 2010, David LaPierre
last reviewed:
Introduction
Elevated core temperature, often, but not necessarily, part of the systemic acute phase response to pathogens or other perceived threats.
Fever enhances hosts immunity, increasing WBC count, decreases iron for bacterial growth, stimulates cytokines. Its duration and degree depend on the severity of the threat and the body's ability to respond.
Body Temperature
Body temperature is the amount of heat produced - heat lost. Internal core temperature is a more reliable indicator than surface temperature, which can change according to the environment or physical activity.
'Core' areas include tympanic membrane, rectum, bladder, esophagus, or pulmonary artery, the most representative.
Recall: C = 5/9 (F-32) F = 9/5 (C+32)
Fever is difficult to define. Basal body temperature varies among people, and also throughout the day.
Normal range of temperature is 36.8 +/- 0.4 for oral temperature.
- rectal 0.6 higher
- axillary 1.0 lower
- varies with circadian rhythm, pregnancy
fever:
- oral >37.8
- axillary >37.4
- tempanic, rectal >38
Fever patterns include:
- sustained: continuously elevated about 38 (100.4o F)
- intermittent: fever spikes interspersed with normal at least once every 24 hours
- remittent: spikes and falls, with no return to normal
- relapsing: fever and normal temperature fluctuations, each potentially longer than 24 hours
- low grade: can also show variations with circadian rhythm
The Case of...
Differential Diagnosis
The differential for fever is extremely extensive, with over 200 causes (Arnow and Flaherty, 1997).
Low grade fever can occur with habitual hyperthermia, chronic fatigue syndrome, or fibromyalgia.
Fever of unknown origin (FUO) is defined as that lasting more than three weeks, with a temperature over 38.3 C on several occasions, and with no identified cause after extensive lab and imaging investigations.
The causes of FUO fall into a number of categories.
infection
- tuberculosis
- malaria
- Whipple's disease
- intra-abdominal abscesses (liver, gall bladder, subdiaphragmatic, kidneys, pelvic organs, psoas)
- babiosis
- Erlichiosis
- Bartonellosis
- Lyme's disease
- Parvovirus B19
- PJP
- prostatitis
- infective endocarditis
malignancy
- lympnomas
- hemoatological malignancy
- cardiac atrial myxoma
miscellaneous
- spondylitis
- pulmonary embolism
- factitious fever
- drug-induced
- habitual hyperthermia
- rheumatic, autoimune, systemic, collagen vascular disease, vasculitides,
- sarcoidosis
- temporal arteritis
- retroperitoneal hematoma
- B12 deficiency
- aortic dissection
- CFS
- alcohol withdrawal
History and Physical Exam
A search for infection is the initial main priority. If a work-up does not initially reveal diagnostic clues, repeated history and physical exam can bring new issues to light over time.
- history
- physical exam
History
History of Present Illness
Past medical history
Medications
|
Family History
Social History
|
Physical Exam
Physical exam should be complete, and should include:
- temporal arteries
- rectal examination
Investigations
There are extensive and expensive investigations available, and their use should be guided in a staged approach, based on potential causes and risks, invasiveness, costs, and sentiments of the patient.
- lab investigations
- diagnostic imaging
Lab Investigations
Blood tests should routinely include:
- CBC
- ESR, CRP
- electrolytes
- renal function tests
- liver enzymes and function tests
- CPK
- LDH
urinalysis
blood culture
urine culture
other cultures (sputum, throat, CSF, pleura, joints) as indicated
tuberculin skin test
For many of the following conditions, the pre-test probability is so low that the positive predictive value of tests will also be low, particularly in regards to IgM.
RF, ANA, other inflammatory antibodies
serology, according to local epidemiology
- HIV
- tuberculosis
- CMV
- EBV
biopsy (liver, bone marrow)
Diagnostic Imaging
Imaging should initially include:
- chest X ray
- abdominal and pelvic ultrasound
Other modalities could include:
- chest r abdominal CT
- echocardiography if murmur present
- endoscopy
- sinus, teeth radiography
- MRI
Whole body tracer scintillography if source continues to be elusive. A number of tracers may be used, including Gallium 67, labeled leukocytes, labeled immunoglobulins, and 18-fluoro-deoxy-glucose.
Management
If no causes are identified after work-up, a number of options are possible:
- watchful waiting
- inflammation tracer scintigraphy
- staged approach
- therapeutic trials
Pathophysiology
Fever, also called pyrexia, is an abnormal rise in body temperature with a sustained oral temperature reading greater than 39.0 ºC. There are three identifiable fever phases.
In the first phase invading pyrogens (bacteria and viruses) trigger immune system responses and cause a rise in body temperature. The hypothalamus reacts by raising the “setpoint” for normal body temperature and the body responds by producing and conserving heat. During the chill phase the person may feel cold and experience chills and shivering, even though the body temperature is rising. The plateau phase of fever occurs when the new setpoint is reached and the person feels warm and dry. If the pyrogens are removed (e.g. antibiotics or antipyretics are initiated) the last phase, or fever break phase, begins with a drop in the hypothalamus setpoint. As the body temperature drops the person becomes warm and flushed due to vasodilation and diaphoresis sets in to assists with heat loss.
If the pyrogens are not removed, a new set point will be set and the body temperature will continue to rise. When the fever “breaks” the person is considered afebrile. It is important to note that the presence of infection is assumed by assessing oral temperatures taken several times during the day, compared with the baseline temperature reading, and correlating signs and symptoms of infection. During a febrile episode, it is also important to assess all vital signs, level of hydration, skin colour, and comfort level.
Acute Phase Response
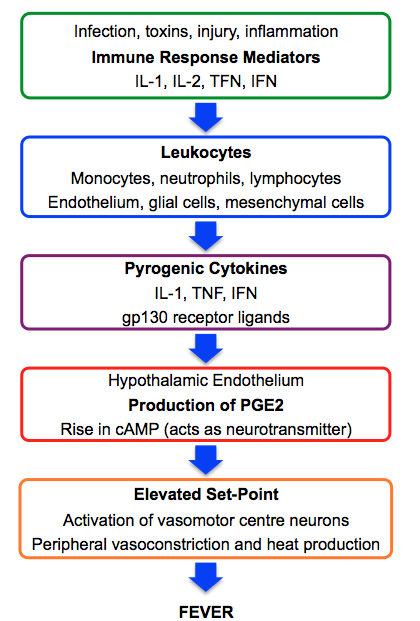
illustrated by Kathryn Dorman
Pyrogens
In response to exogenous pyrogens such as bacterial LPS, leukocytes produce endogenous pyrogens such as IL-1, TNF, and IL-6. These cytokines act on vascular and perivascular cells of the hypothalamus to induce cyclooxygenase, converting AA into prostaglandins. Of these, PGE2 is very important. It induces neurotransmitters such as cAMP to reset the body's temperature set-point. This causes fever, somnolence, and lethargy. It also explains how NSAIDs and acetominophen are antipyrogenic.
The hypothalamus precipitates metabolic and behavioural responses to prostaglandins.
- vasoconstriction, decreased sweating, piloerection, and shivering
- increased metabolism
- increased heart rate and blood pressure
- seeking warmth
- somnolence and malaise
Endocrine and metabolic
- increased glucocorticoids, growth hormone, aldosterone
- decreased ADH, divalent cations
- secretion of cute phase proteins
Defervescence occurs to reduce body temperature. Responses include vasodilation, sweating, and increased ventilation.
Factors affecting body temperature
The very young have difficulties controlling their temperatures, with drastic response to environmental changes; temperature control is unstable till puberty.
The elderly have deterioration of control mechanisms, related to poor vasomotor control, reduced fat stores, reduced sweat gland activity, and reduced metabolism.
Circadian rhythm also leads to changes in body temperature, with changes 0.5-1o in 24 hours. The lowest point is between 1-4 AM, with the highest around 6pm.
Stress increases temp through hormonal and neural stimulation leading to increased metabolism.
Resources and References
Arnow PM and Flaherty JP. 1997. Fever of unknown origin. Lancet. 350(9077):575-80.
Petersdorf RG and Beerson PB. 1961. Fever of unexplained origin: report on 100 cases. Medicine (Baltimore). 40:1-30.
Topic Development
authors:
reviewers:
