
Vulvovaginitis and Vagninosis
last authored: July 2010, Kim Colangelo
last reviewed:
Introduction
A change in vaginal discharge is a frequent presenting complaint. While many cases represent normal changes, numerous infections and other causes may be responsible for discharge. As such, thorough clincial assessment and investigation are required.
Vaginosis is different from vulvovaginitis in that there is no inflammatory reaction, however there is overlap in symptoms between the two conditions.
This topic does not discuss the sexually transmitted infections of Chlamydia and gonorrhea, which are covered in more detail in their own topics.
The Case of Ms. Lyons
A 30yo female presents to her family doctor's office with a 3 day history of a white vaginal discharge. Her main concern is that the discharge smells unpleasant. There is no pruritis, rash, or dysuria. She is otherwise healthy. Gynecological history reveals a past chlamydial infection for which she was treated.
- What are the top 3 things on your differential diagnosis?
- What would your initial next step be?
Causes and Risk Factors
Physiologic discharge can increase during states of increased estrogen, including pregnancy, oral contraceptive pill use, polycystic ovarian syndrome and premenarche.
The three most common causes of vulvovaginitis are bacterial vaginosis, candidiasis, and trichomoniasis.
The main organisms of bacterial vaginosis (BV) include:
The main risk factors for BV include:
|
There are three possible species for candidiasis:
Candidiasis risk factors:
|
Trichomoniasis is caused by Trichomonas vaginalis, which is a flagellated protozoan parasite.
Trichomonas is considered a sexually transmitted infection thus it can be passed between partners.
|
Pathophysiology
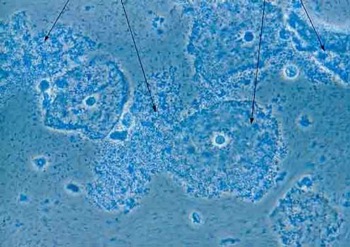
"Clue cells" suggesting bacterial vaginosis
used with permission, Per Grinsted
Bacterial vaginosis
Hydrogen peroxide producing lactobacilli are normally the predominant organism in the vaginal flora. When these decline, the pH rises (become more alkaline) and anaerobes proliferate. The anaerobes produce enzymes that break down substances into amines that have a foul smell; this, combined with the normal cells of the vagina sloughing off more during bacterial vaginosis, results in the discharge that is characteristic.
If Gardnerella vaginalis is the causative organism it can cling to the epithelial cells sloughing off and create the "clue cells" that are part of the diagnostic criteria.
Candidiasis
Candidiasis is a fungal infection. The source may be the perianal area that gains access to the vagina or it may normally be present in the woman and because of altered host factors (such as douching) become symptomatic.
Trichomonas
Trichomonas is considered a sexually transmitted infection. Trichomonas has adherence factors that allow it to adhere to the cervicovaginal epithelium and passed between partners.
Signs and Symptoms
- history
- physical exam
History
History of present illness
- onset
- duration
- previous episodes
- smell, quantity, thickness, texture
- itch, pain
- fever, chills
- associated with intercourse, menstruation, diet, STI?
Obstetric/gyne history
- menarche
- menstruation - regularity, cycle length
- sexual history
- sexually transmitted infections
Past medical history
Medications
Social history
- cigarettes
- alcohol
- drugs
Physical exam
Abdominal exam:
- tenderness
- peritoneal signs
Pelvic exam:
- discharge
- lesions, trauma, rashes
- cervical motion tenderness
- swabs should be taken
Normal (physiologic) discharge is clear or white and odourless.
All three infectious causes may be asymptomatic but seen on cultures.
Condition |
Bacterial vaginosis |
Candidiasis |
Trichomoniasis |
Discharge |
grey, thin, watery, foul smelling, copious |
white, "cottage-cheese" |
yellow-green, foul smelling, copious |
Other symptoms |
discharge is typically the only symptom |
pruritis, dysuria, dyspareunia |
pruritis, dysuria, dyspareunia, burning |
Physical Exam |
copious discharge with no inflammatory reaction |
satellite vulvar erythema swollen, inflamed vulva |
strawberry cervix diffuse vulvar erythema |
Lab Investigations
Normal vaginal discharge, if smeared on a slide, will show epithelial cells (that slough off on a continuous basis) and lactobacilli that are part of the normal vaginal flora. The normal vaginal pH is 3.8-4.2.
Bacterial Vaginosis is diagnosed when at least 3 of the following 4 are present (Amsel criteria):
- thin, watery, grey discharge
- pH >4.5
- fishy odor with 10% KOH (called a whiff-amine test)
- vaginal epithelial cells coated with bacilli (clue cells)
A vaginal culture is not necessary for diagnosing BV or candidiasis; clinical signs and symptoms alone are sufficient. If a swab is taken for the wet mount or pH it should be taken from high in the vaginal canal to avoid contamination with organisms of the skin. The swab can then be applied to a wet mount for the whiff amine test or to look for clue cells, or to litmus paper to check the pH.
Bacterial Vaginosis |
Candidiasis |
Trichomoniasis |
|
KOH |
fishy odour produced |
cells remain intact but no odour is produced |
can be odour producing |
pH |
greatly increased |
normal |
increased |
wet mount
|
clue cells (epithelial cells covered with bacteria) |
budding yeast and hyphae |
oscillating protozoan numerous WBC's and inflammatory cells |
gram stain
|
switch from gram positive rods to gram negative rods or curved bacteria |
gram positive yeast with buds |
large, gram negative protozoan |
Differential Diagnosis
The differential includes:
- atrophic vaginitis (postmenopausal, usually have dyspareunia and signs of inflammation)
- physiologic (cycle related variations in vaginal discharge)
- foreign body
- pinworms
- lichen sclerosis (all more common in prepubertal women)
- local chemical irritation
- trauma
- toxic shock syndrome
- Crohn's disease
Treatments
Bacterial Vaginosis resolves spontaneously in many women so treatment is indicated for symptomatic relief, in pregnant women, and in women about to undergo pelvic surgery.
Some treatment options include:
- vaginal douche with 1.5% hydrogen peroxide
- antimicrobials: metronidazole, tinidazole, or clindamycin; may be given orally, topically, or vaginally
Oral probiotics are currently being investigated as a supplement to antimicrobial therapy, as treatment of BV with antimicrobial therapy may lead to Candida infections.
A male partner does not need to be treated, a female partner should be informed of the infection.
Candidiasis is often treated with antifungals, such as fluconazole A single dose of oral treatment is often preferred for convenience, however suppositories and creams are available. The duration of treatment is lengthened in complicated patients (immunosuppressed, pregnancy, recurrent episodes). Acidophilus yogurt is being investigated to treat candidiasis.
Trichomoniasis should be treated with the antibiotic metronidazole. A single dose of oral treatment is often sufficient. As Trichomonas is a sexually transmitted infection, partners should be treated as well.
Consequences and Course
BV
and trichomoniasis are associated with a higher risk of sexually
transmitted infections such as HIV, HSV, gonorrhea, and chlamydia. They
are also associated with a higher risk of preterm birth and other
obstetric complications in affected pregnant
women and postoperative vaginal cellulitis in women undergoing pelvic
surgery. BV has a high recurrence rate, maintenance antimicrobial
therapy has been investigated. The use of condoms or abstinence has
been associated with lower recurrence rates.
Vaginal candidiasis is not associated with adverse pregnancy outcomes.
Resources and References
Topic Development
authors: Kim Colangelo, 2010
reviewers:
