
Ectopic Pregnancy
last authored: June 2009, Reuben Kiggundu
last reviewed: May 2015, Neerja Sharma
Introduction
Ectopic pregnancy (Greek ektopos, or out of place) refers to the implantation of a fertilized egg outside of the uterine cavity. Ectopic pregnancies frequently rupture, leading to hemorrhage - the leading cause of first-trimester dealth due to pregnancy. Approximately 2% of all first trimester pregnancies are ectopic (ACOG, 2008).

laparoscopic image provided by Dr Charles Hamm
Most ectopic pregnancies - 95-96% - occur in the fallopian tubes, with the majority of the rest being ovarian or cervical.
The abnormally implanted blastocyst grows and draws its blood supply from the site of abnormal implantation. As the gestation enlarges, it creates the potential for rupture and hemorrhage - one of its most dangerous complications.
Causes and Risk Factors
All women of reproductive age are at risk, though rates increase in women over 35.
Black women have the highest rates, followed by non-white and then white women.
Multigravid women have higher rates than nulliparous women.
Anything that hampers the migration of the embryo to the endometrial cavity can predispose to ectopic pregnancy.
- pelvic inflammatory disease - commonly Chlamydia trachomatis (10-15% chance with future pregnancy)
- multiple sexual partners
- history of prior ectopic pregnancy (15-20% recurrence rate)
- prior Caesarean section
- history of tubal surgery and conception after tubal ligation
- use of infertility drugs or assisted reproductive technology
- use of intrauterine devices
- increasing age
- smoking
- salpingitis isthmica nodosa (diverticulosis of the fallopian tube)
- previous DES exposure
- T-shaped uterus
Heterotopic pregnancy, where one embryo is ectopic and the other intrauterine, is on the rise due to increased rates of assisted reproductive technology.
However, over half of all cases of ectopic pregnancy occur in women with none of these risk factors.
Signs and Symptoms
- history
- physical exam
History
The classic clinical triad of ectopic pregnancy includes:
- lower abdominal pain
- amenorrhea
- vaginal bleeding
However, only 50% of patients present typically.
Other symptoms include:
- dizziness, fainting
- passage of tissue
- those common to early pregnancy (nausea, breast fullness, fatigue, heavy cramping etc.)
Inquire into:
- menstrual history (LMP)
- sexual history
- constraceptive use
- gynecologic history (surgery, infections)
Physical exam may reveal:
- unstable vitals: tachycardia, hypotension
- cervical motion tenderness (most frequent sign)
- adnexal tenderness or mass
- abdominal tenderness, rebounding, or guarding
- Cullen sign: blue discoloration around umbilicus suggesting retroperitoneal hemorrhage
- uterine enlargement
- fever
- orthostatic hypotension
Vaginal bleeding is usually minimal, compared to that seen with spontaneous miscarriage.
Investigations
- lab investigations
- diagnostic imaging
Lab Investigations
When considering ectopic pregnancy, the following may be helpful:
- beta-HCG: quantitative testing can be done at 48h intervals; it normally doubles in this time with intrauterine pregnancy, and will rise more slowly with ectopic pregnancy
- serum progesterone may distinguish between viable and nonviable pregnancy
In order to assess stability, and prepare for treatment, consider:
- CBC
- Rh type
- crossmatch
Diagnostic Imaging
Transvaginal ultrasound (TVUS) is the preferred modality to identify extrauterine pregnancy. A gestational sac is typically visible, regardless of location, if beta-HCG is more than 1500 IU. However, a negative ultrasound does not exclude ectopic pregnancy.
Ectopic findings include:
- complex adnexal mass
- fluid-filled adnexal mass
- free fluid in the peritoneal cavity
- gestational sac in the cornual area
- intracervical location
CT, MRI, or Doppler flow may also be done, though are not as helpful.
Differential Diagnosis
Other possible conditions include:
- normal pregnancy
- appendicitis
- urinary tract infection
- ovarian torsion
- ovarian cyst
- salpingitis
- ruptured corpus luteum cyst
- threatened abortion
Pathophysiology
Damage to the cilia in Fallopian tubes is frequently responsible for ectopic pregnancy, caused by factors such as pelvic inflammatory disease (PID) or surgery.
Treatments
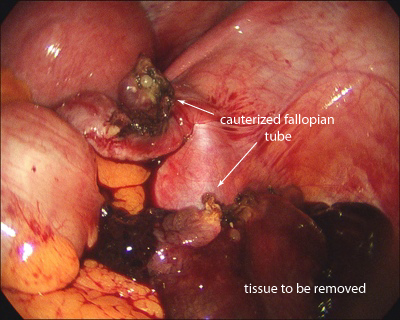
laparoscopic image provided by Dr Charles Hamm
Initial focus should be on the ABC's to stabilize the patient:
- oxygen as needed
- two large bore IVs and fluid resuscitation
- CBC and cross-match
Rhogam should be given as appropriate.
Medications
Methotrexate is the primary nonsurgical treatment. It can be used in situations of:
- stable patient
- no signs of active bleeding
- patient can be trusted to follow-up
Indications include:
- unruptured mass <3.5 cm
- no fetal activity
- desire for future fertility
- beta HCG <5000 IU
Contraindications include:
- active intraabdominal hemorrhage
- breast feeding
- immunodeficiency
- alcoholism
- chronic hepatic, renal, or lung disease
- blood dyscrasias
- peptic ulcer disease
Surgery
If surgery is warranted, laparascopy followed by salpingectomy or salpingostomy is the preferred approach. Open laparotomy is mandated if the patient is unstable..
Consequences and Course
Ectopic pregnancy can lead to massive hemorrhage, infertility, and death.
Between 25-30% of women will have another ectopic pregnancy if they conceive.
Prevention of STIs, especially Chlamydia, may reduce incidence of ectopic pregnancy.
Resources and References
Murray H et al. 2005. Diagnosis and treatment of ectopic pregnancy. CMAJ. 173(8).
ACOG Practice Bulletin. 2008. Number 94: Medical management of ectopic pregnancy.
