
Appendicitis
last authored: Feb 2015, David LaPierre
last reviewed:
Introduction
Appendicitis is an acute condition which occurs as a result of inflammation of the appendix. It is relatively uncommon, but can be extremely serious and even life-threatening. In 2013, 72,000 people died globally from appendicitis (GBD, 2015).
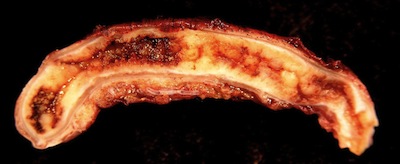
Inflamed appendix, used with permission
The appendix is a small tube, closed at one end, which is found at the junction between the small and the large intestine. It has no known function in digestion. The appendix can become inflamed when the lumen becomes obstructed. This is often caused by partially digested food, but can also be related to fecal material, parasites, swallowed bodies, and lymphoid hyperplasia.
Effective diagnosis of appendicitis is difficult at times, especially without adequate lab and imaging capability. An important consideration is to proceed to surgery - appendectomy - for the appropriate patients. Observation with medical management may be feasible in some settings, but surgical availabilty is essential for safe care.
The Case of Fred W.
Fred is a 22 year-old man. He wakes up after a late night out on the town with mild abdominal pain. He initially ignores it, but as the pain worsens and he develops nausea, vomiting, and fever, he decides to go to the local clinic.
- Q: what should you be concerned about?
- Q: how do you assess for possibility of appendicitis?
Causes and Risk Factors
Acute appendicitis commonly affects adolescents and young adults, but it can occur at any age.
Acute appendicitis results from bacterial infection of the appendical wall, usually distal to an obstruction of the lumen. The obstruction is caused by:
- faecaliths
- seeds or other particulate food matter
- worms in the lumen
- invasion of the appendix wall by parasites, such as amoeba or schistosoma
- lymphoid hyperplasia following a viral infection
Pathophysiology
When pressure increases, venous flow is obstructed and blood flow ceases. Ischemia is accompanied by anaerobic bacteria proliferation. Transmural inflammation can follow.
Signs and Symptoms
As described, clinical diagnosis can be difficult at times. For many patients, specific signs or symptoms can make the diagnosis more likely, but unfortunately, an absence of signs or symptoms does not rule it out.
- history
- physical exam
- scoring systems
History
Pain often begins with vague peri-umbilical discomfort, progressing to right lower quadrant pain. This pain may be burning in nature.
Anorexia, nausea and vomiting may be present. The absence of pain before vomiting reduces the likelihood of appendicitis.
Fever is common, particularly as inflammation progresses.
Asking about pain when traveling over speed bumps has a sensitivity of 97%, but a specificity of only 30% (Ashdown et al, 2012).
Physical Exam
The patient may look uncomfortable and unwell.
Vitals may include:
- tachycardia
- fever
- hypotension if shock is developing
However, note carefully that vitals can be normal in early appendicitis!
A full abdominal exam should be done. Specific maneuvers assessing for appendicitis include:
- right lower quadrant (RLQ) tenderness, guarding, or rigidity
- percussion tenderness
- RLQ pain after pressure in the LLQ
- RLQ tenderness on rectal examination
Peritoneal involvement leads to reduced movement and guarding or rigidity of the abdominal muscles. An acute abdomen may result.
The psoas sign occurs with abdominal pain with resisted flexion of the hip. This movement activates the psoas, irritating an inflamed appendix and surrounding tissues.
An internal exam should be performed in women, assessing for gynecological causes of abdominal pain.
Scoring Systems
The Alvarado score assists in guiding diagnosis (REF).
Finding |
Points |
Finding |
Points |
pain migrating to RLQ |
1 |
rebound pain |
1 |
anorexia |
1 |
elevated temperature |
1 |
nausea/vomiting |
1 |
leukocytosis |
1 |
RLQ tenderness |
1 |
WBC left shift |
2 |
If <4 points, very low risk
If <7 lower risk
If 7 or greater, 50% probability
The Ohmann score is another tool that may be used.
Investigations
- lab investigations
- diagnostic imaging
Lab Investigations
Bloodwork may include:
- complete blood count, including WBC differential
- liver function tests
- creatinine
- electrolytes
- amylase and lipase (if pancreatitis is suspected)
- urinalysis for hematuria, infection
- pregnancy test
- stool for c &s, ova and parasites
Diagnostic Imaging
Decision to pursue imaging should follow clinical assessment.
Low risk individuals may be observed.
Medium risk individuals may be imaged.
High risk patients should proceed to surgery, without imaging.
Imaging modalities to consider include:
- ultrasound - helpful in making diagnosis
- CT - helpful in making diagnosis
- abdominal X ray - helpful in assessing other causes of acute abdominal pain
Differential Diagnosis
Discriminating appendicitis from other causes of abdominal pain is important but also difficult, especially early on during the disease course.
Other causes of abdominal pain are described for children and for adults.
Treatments
If appendicitis is suspected, rapid and careful assessment should be done in a centre with surgical capability. Small sips of water may be offered, along with pain-relieving medicine, but the patient should be advised not to eat or drink, in anticipation of surgery.
An IV should be started to provide fluid resuscitation and balancing of electrolytes.
An appendicular mass may be treated with medical management, with close observation for worsening.
An appendicular abscess may be treated with medical management, along with incision and drainage.
An acute, perforated, or gangrenous appendix should be treated with appendectomy.
Surgical technique is described in the WHO's publication, Surgical Care at the District Hospital.
Consequences and Course
Appendicitis can cause:
- local peritonitis
- abscess formation
- gangrene of the appendix
- perforation
general peritonitis
Appendicitis can rapidly be lethal if the infection spreads from the peritoneal cavity to the blood stream, resulting in sepsis.
Surgical removal of the inflamed appendix, particularly if perforation has not occurred, normal results in rapid and complete recovery.
Resources and References
Ashdown HF, D'Souza N, Karim D, Stevens RJ, Huang A, Harnden A. 2012. Pain over speed bumps in diagnosis of acute appendicitis: diagnostic accuracy study. BMJ. 345:e8012.
GBD 2013 Mortality and Causes of Death, Collaborators. 2015. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. 2015. Lancet. 385(9963):117-171.
Hardin DJ. 1999. Acute Appendicitis: Review and Update. AFP. 60(7):2027-2034.
Topic Development
authors:
reviewers:
