
The Stomach
last authored: May 2011, Eric Leung
last reviewed: June 2011, Kelvin Leung
Introduction
The stomach is a pear-shaped organ part of the gastrointestinal (GI) tract that functions in digesting food, absorbing its nutrients, and excreting wastes. The stomach functions to store, dissolve, and partial breakdown macromolecules. The glands of the stomach secrete a strong acid, hydrochloric acid (HCl), and protein-digesting enzymes. The stomach acid also serves to kill bacteria entering the organ.
The gastric mucosa is vulnerable to damage, but is protected by high turnover, tight junctions, mucus, and bicarbonate (HCO3-) secretions. For example, the high turnover is demonstrated by cells on either side are capable of switching from columnar to squamous and fill in the hole within a few hours following a gastric biopsy. Failure of any of the above protective mechanisms can lead to gastric bleeding.
The main function of the stomach is to store, mix, dissolve, and continue the digestion of food in addition to regulating its emptying of its contents into the small intestine. Its mucus secretions also help protect the stomach from the acid that it produces to activate pepsinogen to pepsin and kill microbes that enter the body. The food mixture resulting from the digestion in the stomach is known as chyme, comprised of protein and polysaccharide fragments, fat droplets, salt, water, and various other molecules ingested.
Anatomy
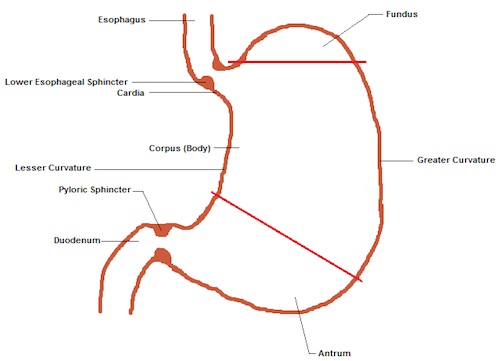
Stomach anatomy, illustrated by Eric Leung
As food passes through the esophagus, it reaches the cardia, the junction at which the esophagus attaches to the stomach. The cardia secretes mainly mucus and HCO3-. Passing through the lower esophageal sphincter, the food will then enter the stomach which is comprised of 3 parts: the fundus, corpus (body), and antrum.
The fundus is the most superior portion of the stomach; superior to the fundus is the diaphragm and lateral to it is the spleen.
The right (medial) side of the corpus is relatively straight and is known as the lesser curvature while the left (lateral) side of the corpus is known as the greater curvature. The lesser curvature is attached to the liver by the hepatogastric ligament. The cells most commonly found in the fundus and the corpus are the parietal, chief, enterochromaffin-like (ECL), and D cells.
The most distal portion of the stomach is the antrum which comprises about ¼ of the stomach and largely contains G cells and D cells. Distal to the antrum is the pyloric sphincter which connects to the beginning of the duodenum of the small intestine.
Cell Biology
- parietal
cells - interstitial
cells of Cajal - G cells
- D cells
- chief
cells - enterochromaffin-like
cells - mucus neck
cells
Parietal Cells
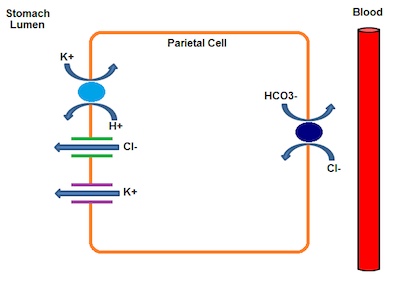
Parietal cell function, illustrated by Eric Leung
The majority of stomach parietal cells reside in the corpus. Parietal cells secrete HCl in response to gastrin from G cells, histamine from ECL cells, or acetylcholine (ACh) from the vagus nerve. It can also be stimulated by protein ingestion, distension of the stomach, or even the thought of food. Secretion of stomach acid is negatively regulated by somatostatin.
The primary transporter responsible for the acidity of the stomach is the H+/K+ ATPase, which is located on the apical surface of the cell. Parietal cells secrete a proton (H+) into the lumen of the stomach in exchange for a potassium ion (K+) into the parietal cell. The H+/K+ ATPase pumps against a H+ concentration gradient of over 1 million:1. HCl is formed when chloride ions (Cl-) passively flow out through the Cl- channels into the lumen to maintain electroneutrality. The source of Cl- ions comes from a Cl-/HCO3- exchanger. Blood CO2 and H2O produce HCO3- and H+ through the enzyme carbonic anhydrase. The HCO3- is secreted into the interstitial fluid (which enters the blood) in exchange for Cl- ions into the parietal cell. Thus, an alkaline tide can induce alkalosis in a person with extreme H+ secretion.
Drugs such as omeprazole and esomeprazole (proton pump inhibitors) can irreversibly inhibit the H+/K+ ATPase at low pH but not at neutral pH. Therefore, it is able to prevent excessive secretion of stomach acid.
Additionally, cimetidine (histamine H2 receptor antagonists) can inhibit the H+ secretion induced by histamine as well as the indirect effects of ACh- and gastrin-induced H+ secretion.
Parietal cells also secrete a glycoprotein, intrinsic factor, which binds to vitamin B12. Vitamin B12 is not intrinsically synthesized by mammalian cells; humans obtain vitamin B12 consumption of meat, fish, and dairy products which are released by the acidic environment and pepsin in the stomach. Another glycoprotein known as haptocorrin (factor R), produced by salivary and gastric glands, binds to vitamin B12 in the stomach. Proteases from the pancreas digest factor R, freeing vitamin B12 and allowing it to complex with intrinsic factor in the duodenum. Receptors on epithelial cells of the ileum bind this complex and endocytose it. Deficiency in vitamin B12 can lead to a condition called pernicious anemia; this can be treated by intramuscular injections of the deficient vitamin.
Interstitial Cells of Cajal
These are known as the pacemaker cells of the gastrointestinal tract which provides the gut with a basic electrical rhythm that spreads to nearby smooth muscle cells. The purpose of these cells is to elicit the depolarization of smooth muscle cells, resulting in contraction and relaxation and leading to the mechanical breakdown of food for emptying into the duodenum. Each segment of the gut has its own slow wave frequency. For example, the frequency in the stomach is approximately 3 per minute while it is approximately 10-12 per minute in the small intestine. In the stomach, these cells along the greater curvature provide the dominant rhythm because they pace most frequently.
The frequency of these slow waves determines the maximum rate at which the smooth muscle contracts because action potentials can only occur on top of these rhythmic pulses. Normally these changes do not reach the threshold for contraction. However, with stimulation from the vagus or hormones such as gastrin, the threshold is crossed and contraction occurs. Contraction strength increases with stimuli strength, but there is no change in contraction frequency.
The slow waves do not propagate into the small intestine because there is an electrically quiescent region between the pyloric sphincter and duodenum that does not conduct this electrical signal.
G Cells
G Cells, which are located in the antrum, produce gastrin in response to the partially digested peptides, stomach distension, or gastrin-releasing peptide (GRP). Gastrin is a peptide hormone that binds to cholecystokinin (CCK) receptors on parietal cells, stimulating H+ secretion.Gastrin also induces antral motility and mucosal growth. Thus, a problem arises when there is excessive production of gastrin, for example by tumor cells, leading to a condition called Zollinger-Ellison syndrome. This condition is characterized by excess acid in the small intestine which leads to mucosal damage, and fatty diarrhea (steatorrhea) due to inactivation of pancreatic lipases.
D Cells
Somatostatin is a peptide hormone secreted by D cells located in the antrum and corpus that inhibits gastric acid secretion from parietal cells. Normally, H+ is sensed by the D cells in the antrum which leads to the secretion of somatostatin and inhibition of the adjacent G cells, leading to less gastrin production and subsequently, less acid secretion. The parietal and ECL cells are also inhibited as well. This provides negative feedback regulation for stomach acid secretion.
Chief Cells
Also known as zymogenic cells which are located in the corpus, they secrete pepsinogen (a zymogen), that is activated by HCl in the stomach lumen to pepsin. Pepsinogen is activated when the pH drops below 5.0 and its optimal pH is about 2.0. Acetylcholine (ACh) is the major stimulator of pepsinogen secretion while other factors such as gastrin also participate. Pepsin is an endopeptidase responsible for the initial digestion of proteins to peptides - approximately 10% of total protein digestion.1
Enterochromaffin-like Cells
These cells are usually located close to parietal cells, producing histamine that act in a paracrine fashion to activate H2 receptors thereby stimulating gastric acid secretion. These cells are stimulated by gastrin and ACh.
Mucus Neck Cells
Mucins and bicarbonate are secreted by these surface epithelial cells located in the corpus and antrum. Mucins are high molecular weight molecules that have oligosaccharide chains that expand when hydrated in the stomach, giving the mucus its viscoelastic qualities. They also combine with HCO3- and phospholipids to form the protective gel of the stomach. The HCO3- secreted into the gel is able to maintain the pH at about 7.0. One of the major stimulators of mucus secretion is prostaglandins, which can be inhibited by non-steroidal anti-inflammatory drugs (NSAIDs).
Chronic use of NSAIDs such as ibuprofen or Aspirin (acetylsalicylic acid) can increase a person's risk of mucosal ulceration. One drug that can be used to counter the effects of NSAIDs is misoprostol, a synthetic prostaglandin.
Development
The gastrointestinal tract is derived from the endoderm. The embryonic gut is an endodermal tube surrounded by mesoderm which appears during the 3rd week of the embryonic stage. This endodermal or digestive tube, which later develops into the stomach and intestines, is suspended by a ventral and dorsal mesentery where the liver and pancreas will later grow into in the 4th week of development, respectively. The ventral mesentery becomes the lesser omentum while the dorsal mesentery develops into the greater omentum.
Resources and References
Topic Development
authors: May 2011, Eric Leung
reviewers: June 2011, Kelvin Leung
