Dialysis
last authored: March 2009, David LaPierre
last reviewed:
Introduction
Dialysis is the removal of waste products and excess fluids following acute or chronic renal failure. There are three types of dialysis - hemodialysis, hemofiltration, and peritoneal dialysis (PD). At best, dialysis provides an average clearance of 10 ml/min, compared with a normal GFR of 120 ml/min.
Indications
Indications include:
- GFR <5-10 ml/min
- BUN >30mmol/L
- hyperkalemia refractory to medical management
- acidosis, refractory to medical management
- fluid overload, refractory to medical management
- uremia: pericarditis, encephalopathy, seuzures, bleeding
- poisonings: ASA, methanol, ethylene glycol, lithium, TCAs, theophylline
- hypercalcemia?
- Acidosis
- Electrolytes
- Ingestion
- Overload
- Uremia
During dialysis, urea, phosphate, and other things are taken out, while calcium and bicarbonate added back in.
A semi-permeable membrane filters dialysate solution to regulate fluid and electrolyte balance.
Types of Dialysis
- peritoneal dialysis
- hemodialysis
- hemofiltration
- choosing the right type of dialysis
Peritoneal Dialysis

Peritonaeal dialysis (PD), as the name suggests, uses the peritoneal membrane's semi-permeable characteristics to filter wastes and provide fluid and electrolyte homeostasis.
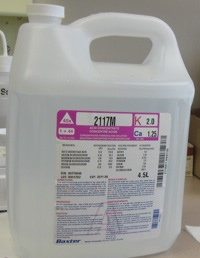
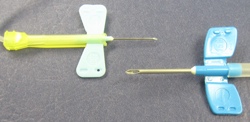
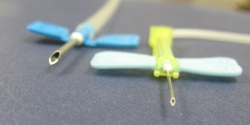
PD uses a permanent catheter, inserted through the abdomenal wall, to transfer fluid to and from the peritoneal cavity. The catheter, shown at left, has multiple holes to increase fluid passage.
Dialysate is tranferred up to 5 times daily, with fresh fluid introduced each time. Solutes move down their concentration gradients, while water is shifted via osmotic drag, provided by dextrose or other solutes.
When starting PD, the quality of a person's membrane is unknown. Perfusion rates are controlled by surface area, vasculature, and amount of peritoneal scarring, and emperic approaches are used to plan future treatments.
Dialysate comes in various concentrations, ie 0.5%, 1.5%, 2.5%, or 4.25%. Concentration used on a given day depends upon fluid status - weight gain/loss, peripheral edema, blood pressure, or symptoms thereof.
PD is used in various settings, including as maitenance for end-stage renal failure. Technique survival decreases to 50% after 5 years due to loss of peritoneal membrane function.
Complications include:
- peritonitis (often due to Staph. epidermidis). Treatment is with intraperitoneal or intravenous antibiotics.
- mechanical blockage of fluid drainage, often by constipation
- infections at catheter site
- pleural effusions or sclerosing peritonitis
Contraindications include:
- peritoneal adhesions following peritonitis
- abdominal hernia
- colostomy
It is important to assess the bag of spent dialysate. Look at clarity, presence of fibrin, and bag weight to learn how much fluid was taken off.

 Blood flows through the many tubes in the filter, shown on the right. The tubes, composed
of semi-permeable membranes, are bathed in dialysate fluid, and fluid
and solutes pass through the tubes bi-directionally. Blood then flows
out the bottom of the filter before being returned to the body.
Blood flows through the many tubes in the filter, shown on the right. The tubes, composed
of semi-permeable membranes, are bathed in dialysate fluid, and fluid
and solutes pass through the tubes bi-directionally. Blood then flows
out the bottom of the filter before being returned to the body.