


Low risk drinking is defined as 2 or less drinks per day, with 9 or less drinks weekly for women and 14 or less weekly for men.
At least 10-15% of the adult population in Canada are problem drinkers.
Over 500,000 Canadians are alcohol-dependent.
20-50% of hospital admissions, 10& of premature death, 30% of suicides, and 50% of traffic fatalities in Canada arealcohol-related.
22% of people aged 25-35 who drink have five or more drinks on a typical day.
Alcohol withdrawal can be significant and life threatening, and can be treated with benzodiazepines.
In 2002, liver cirrhosis was most common cause of death caused by alcohol.
Each year, over 4 million Canadians drive while drunk.
Impaired drivers account for 29% of driver fatal
Smashed - Transport Canada publication on drinking and driving.
Ethanol is metabolized in the liver by two oxidation reactions.

A massive increase in NADH results, and this diverts pyruvate and OAA away from gluconeogenesis.
This, accompanied by potential reduced dietary intake and depletion of the liver's glycogen stores, can result in hypoglycemia.
Many of the behavoiurs associated with alcohol intoxication - agitation, impared judgement, and combativeness - can be produced by hypoglycemia.
The acute depressive effects of alcohol are thought to be due to changes in the fluiditiy of membrane phospholipids and altered signal transduction.
Ethanol acts on GABAA receptors in the brain to cause its sedative/hypnotic effects.
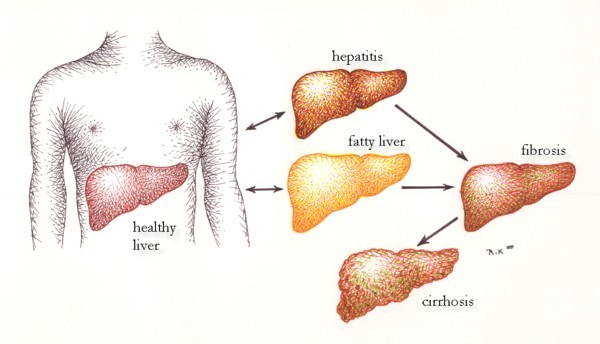
Alcohol causes acute, reversible fatty liver, which in chronic alcoholics can lead to palpable hepatomegaly. Breakdown of peripheral fat stores leads to increased free fatty acids in the liver, and lipid biosynthesis is increased due to excess NADH production. As well, fatty acid oxidation is decreased.
Acute alcoholic hepatitis is much more serious but is also potentially reversible. It can lead to fever, liver tenderness, and jaundice. Ethanol and its metabolites are directly toxic to hepatocytes, leading to necrosis and fibrosis.
In chronic ethanol use, 10-15% of alcoholics develop cirrhosis, characterized by a hard, shrunken liver. The threshold for cirrhosis is and 40-80g/day for men, lower for women, for 10-20 years. Cirrhosis is a serious, potentially fatal disease accompanied by weakness, muscle wasting, ascites, GI hemorrhage, and coma.
Chronic thiamine deficiency is common in alcoholics and leads to nerve cell degeneration, reactive gliosis, and cerebellar and nerve atrophy. This leads to the ataxia, altered cognition, and nystagmus of Wernicke syndrome. Severe memory loss can also accompany alcohol use, termed Korsakoff syndrome.
Ethanol-induced secretion of catecholamines can lead to hypertension.
Chronic alcohol use can cause cardiomyopathy, and while the mechanism is unknown, direct toxicity is likely involved.
Ethanol toxicity can lead to acute gastritis, and chronic users can develop acute and chronic pancreatitis. This may lead to vitamin deficiencies through a loss in pancreatic enzymes.
Oral/esophageal cancer can also be caused by alcohol consumption.
Chronic alcoholism often leads to reduced availability of vitamins due to dietary and liver insufficiency. Thiamine insufficiency (wernicke-Korsakoff Syndrome) is common, leading to peripheral vasodilation and myelin degeneration. Thiamine is involved in the oxidative decarboxylation of pyruvate and alpha-ketoglutarate, two important molecules in energy metabolism.
Ethanol can be toxic to skeletal muscle, leading to muscle weakness, pain, and breakdown of myoglobin.
Alcohol can lead to testicular atrophy and decreased fertility, both in men and women.
Fetal alcohol syndrome is a tragic consequence of alcohol during pregnancy.
Anemia and coagulopathies can be linked to alcohol.
Alcohol is associated with cancers of the mouth, pharynx, esophagus, liver, and possibly the breast. Upper GI cancers may result from the reduction in detoxification of carcinogens such as nitrates and nitrites.
Methanol is metabolized into formaldehyde, resulting in metabolic acidosis, dizziness, vomiting, blurred vision and blindness, and respiratory depression.
Insomnia, trauma, family violence, anxiety, depression, sexual dysfunction, and social/family problems can be caused or worsened by alcohol.
Alcohol abuse and addiction is of serious concern for us all.
Drinking above low-risk levels, but with no alcohol-related physical or social problems, puts people at risk.
Alcohol abuse is defined as levels above low-risk drinking, with one or more of:
Two or more for men, or one or more for women, suggest need for further assessment.
WHO AUDIT tool for primary care.
A positive response on any one of the RAPS4 items or both of the QF items is considered positive on the RAPS4-QF.
The RAPS4-QF added the two QF items:
Conjunctival injection. The condition of the conjunctival tissue is evaluated on the basis of the extent of capillary engorgement and scleral jaundice. Examination is best conducted in clear daylight by asking the patient to direct his gaze upward and then downward while pulling back the upper and lower eye-lids. Under normal conditions, the normal pearly whiteness is widely distributed. In contrast, capillary engorgement is reflected in the appearance of burgundy-coloured vascular elements and the appearance of a greenish-yellow tinge to the sclera.
Abnormal skin vascularization. This is best evaluated by examination of the face and neck. These areas often give evidence of fine wiry arterioles that appear as a reddish blush. Other signs of chronic alcohol ingestion include the appearance of 'goose-flesh" on the neck and yellowish blotches on the skin.
Hand tremor. This should be estimated with the arms extended anteriorly, half bent at the elbows, with the hands rotated toward the midline. Can also be caused nervousness, neurological disorder, nicotine, or caffeine.
Tongue tremor. This should be evaluated with the tongue protruding a short distance beyond the lips, but not too excessively.
Hepatomegaly. Hepatic changes should be evaluated both in terms of volume and consistency. Increased volume can be gaged in terms of finger breadths below the costal margin. Consistency can be rated as normal, firm, hard, or very hard.
Several laboratory tests are useful in the detection of alcohol misuse.
False positives can occur when the individual uses drugs (such as barbiturates) that induce GGT.
While relapse is common, 25-30% of people who abuse alcohol will improve on their own.
With treatment, 60-70% of people with jobs and families have an imprived quality of life after one year.
Inverventions should be consistent with motivation for change.
Regular follow-up is crucial.
Outpatient/day programs for people with chronic problems
Inpatient programs can be useful if people need detoxification, have severe medical/psychiatric problems, have a dangerous or unstable home environment, or have had difficulty with other treatment programs.
Diazepam should be used to manage alcohol withdrawal.
Disulfiram (Antabuse) blocks conversion of acetaldehyde to acetic acid. Its buildup leads to flushing, headache, nausea, and hypotension if alcohol is ingested, discourages alcohol abuse. Depending on country, it can be hard to obtain.
Naltrexone is a competitive opioid antagonist. It reduces cravings and the pleasurable aspects of alcohol. However, it will inactivative prescription opioids as well, and can trigger opioid witdrawal.
Increase HDL levels and decrease platelet aggregation at moderate levels.