
Nasogastric Tube
last authored: Dec 2009, David LaPierre
Introduction
Nasogastric intubation has a number of therapeutic and diagnostic applications. While generally considered a basic medical procedure, it frequently involves some degree of discomfort for the patient. This discomfort may be reduced through proper preparation and the use of topical anaesthetics in patients who are awake.
Serious complications, while uncommon, often occur as a result of incorrect and unrecognized misplacement of the tube in an unconscious patient. Special care to clinically and radio-graphically confirm tube placement in these patients is warranted.
Indications and Contraindications
- indications
- contraindications
Indications
Indications of NG tube placement include:
- relief of gastrointestinal obstruction or ileus, i.e. Mechanical bowel obstruction or following abdominal surgery
- administration of medications or enteral feeding - when the patient is unable to swallow
- diagnostic or motility studies i.e. ph monitoring or to determine the motor activity of GI tract
- obtain specimen of gastric contents for diagnostic purposes, i.e. pyloric or intestinal obstruction
- gastric lavage for overdose in some centers
- diagnosis and therapy of upper GI bleeding (controversial)
When the purpose of NG tube placement is to apply suction/decompression to the GI tract, this is best performed using an intermittent suction device (ie Gomco Suction). Constant, high suction may draw gastric mucosa into the catheter tip and cause mucosal injury.
In addition, nasogastric fluid losses should be documented by the nursing staff. Because nasogastric fluid losses can be significant, IV replacement may be required. A typical replacement solution would be (0.45 NaCl with 10mEq KCl per liter).
Contraindications
Contraindications include:
- recent (past 30 days) nasopharyngeal, Upper GI surgery, esophageal surgery - esophageal rupture may be fatal.
- suspected basal skull (cribiform plate) fracture - the tube is rigid enough to pass directly into the cranial vault rather than the esophagus!
- severe maxillofacial trauma
- thermal or chemical injury to upper respiratory tract or esophagus
- esophageal or nasal pharyngeal obstruction
- coagulopathy (Relative contraindication) - nosebleeds (epistaxis) in these circumstances may be difficult to control
Materials Required
NG tubes are flexible tubing ~ 60 - 100 cm long with multiple drainage holes at the distal end. They generally have markings on the side to assist in judging the correct length of insertion. (Fig 2.1)
Types of NG tubes
Levine catheter: single lumen, small bore
- more appropriate for administration of medication/nutrition
Salem Sump catheter: double lumen (aspiration + venting), large bore
- more appropriate for aspiration
- venting reduces negative pressure and
prevents gastric
mucosa from being drawn into catheter
You will also require:
- gloves (non-sterile) and eye wear
- nasogastric Tube(s) - Adults typically 14 - 18 French
- water soluble lubricant or Xylocaine Jelly
- Xylocaine Spray
- Glass of water
- Tape
- Kidney basin
- Stethoscope
- Suction Apparatus (suction applications only)
Tube diameter increases numerical size. A 14-18 French Catheter is typically used for suction, while enteral feeding tubes may be smaller (8 French). In general, the largest tube which can be comfortably accommodated is chosen - larger tubes are less
likely to become blocked.
Procedure
© 2006-2007. PocketSnips (http://www.pocketsnips.org).
Video - Nasogastric tube insertion. Not a substitute for medical advice.
Introduce yourself, explain the procedure to the patient and obtain verbal consent. Take a history to determine patient’s allergies, medications, indications, and contraindications of this procedure.
Position the patient comfortably - sitting upright with the back and head supported, if possible.
Put on protective eyewear and gloves.
Examine the patient’s nose for patency or septal deviation. Choose the side which seems most patent. Anesthetize with Xylocaine spray if patient not allergic.
Estimate the appropriate insertion distance as shown below - from lips, around ear, and to xyphoid process at base of sternum.
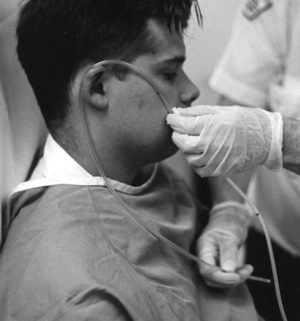
image from Dalhousie University,
Learning Resource Centre
Lubricate the tip of the catheter.
Ask the patient to tilt their chin towards their chest.
Place the tip of the catheter inside the chosen nostril and advance it gently backwards, parallel to the floor of the nasal cavity. Do not force against resistance or patient discomfort.
Some minor resistance may be felt as the catheter tip turns downwards and enters the
nasopharynx. The patient should then be able to feel the catheter tip in the pharynx and may gag.
Have the patient take small sips of water as you further advance the catheter into the esophagus
Stop when the catheter has reached the predetermined insertion distance.
Confirm tube placement in two ways:
- fill the 60 cc syringe with air and attach it to the flared end of the NG Tube. Slowly push the air into the tube while auscultating the patient’s epigastrium. A bubbling noise confirms correct catheter placement
- aspirate from the flared end of the tube using the catheter tip syringe - look or stomach contents.
Once you are happy with the tube position, tape the tube to the patient’s nose. A mark or piece of tape is to be placed on the tube at the entry point to the nare. This is an assessment indicator of possible tube migration.
Chest x-ray confirmation of placement is mandatory prior to instilling material such as medications or tube feedings down an NG tube.
Patients who have known or suspected basal skull (cribiform plate) fractures, recent nasopharyngeal surgery or coagulopathy should have gastric tubes placed orally.
Troubleshooting
Nasogastric intubation is generally uncomfortable. It is a good policy to use topical anaesthetics to reduce patient discomfort.
Tube placement must be confirmed with a chest x-ray, aspiration and auscultation when:
- medications or feeds are to be given
- tracheal/bronchial passage of an NG tube causes coughing and inability to speak in an awake patient
- in an ill or semi-conscious patient
- NG tube placement is difficult
Complications
- epistaxis (common)
- local trauma or irritation to the nasopharynx (common)
- endobronchial placement - uncommon in awake patients. May be hard to recognize in a patient with depressed level of consciousness.
- sinusitis or otitis media - more common with prolonged treatment
- esophageal injury or perforation - rare but potentially fatal
Test Yourself
Question 1
A 32 year-old man took an overdose of diltiazem and promptly walked in front of an SUV. He is brought in to the emergency department 20 minutes later by ambulance, semi-conscious and moaning in pain. Primary survey reveals a heart rate of 124, a blood pressure of 74/56, and a respiratory rate of 22. Secondary survey shows scalp laceration and facial bruising, obvious fractures to his left humerus, and abdominal brusing. He coughs up some frothy blood as you examine him.
The emergency room doctor asks you to insert an NG tube to begin gastric lavage for his overdose.
Which of the following is his contraindication to NG tube placement?
A: semi-conscious state
B: unstable vital signs
C: two black eyes
D: abdominal bruising
E: hemoptysis
answer (hover mouse for answer)
Question 2
Additional Resources
