
Human Papilloma Virus
last authored:
last reviewed:
Introduction
Human papillomavirus (HPV) causes frequent infections in humans. It is the most common sexually transmitted infection, causing genital and anal warts and various malignancies, most notably cervical cancer. HPV is also responsible for warts occurring on the hands and feet.
Papilloma, Alison Martin, 2010
The Case of...
Epidemiology
Classification and Characteristics
Transmission and Infection
HPV is passed on through genital contact, most often during vaginal and anal sex. HPV may also be passed on during oral sex and genital-to-genital contact. HPV can be passed on between straight and same-sex partners—even when the infected partner has no signs or symptoms.
A person can have HPV even if years have passed since he or she had sexual contact with an infected person. Most infected persons do not realize they are infected or that they are passing the virus on to a sex partner. I
It is also possible to get more than one type of HPV. Very rarely, a pregnant woman with genital HPV can pass HPV to her baby during delivery. In these cases, the child can develop Juvenile-Onset Recurrent Respiratory Papillomatosis (JORRP).
It is thought that the HPV virion infects epithelial tissues through micro-abrasions, whereby the virion associates with putative receptors such as alpha integrins and laminins, leading to entry of the virions into basal epithelial cells through clathrin-mediated endocytosis and/or caveolin-mediated endocytosis depending on the type of HPV.
The HPV life cycle follows that of infected keratinocytes.
The viral genome is transported to the nucleus and establishes itself at a copy number between 10-200 viral genomes per cell. A sophisticated transcriptional cascade then occurs as the host keratinocyte begins to divide and become increasingly differentiated in the upper layers of the epithelium.
E6/E7 proteins
The viral oncogenes, E6 and E7 are thought to modify the cell cycle so as to retain the differentiating host keratinocyte in a state that is favourable to the amplification of viral genome replication and consequent late gene expression. E6 in association with host E6 associated protein, which has ubiquitin ligase activity, act to ubiquitinate p53, leading to its proteosomal degradation.
E7 (in oncogenic HPVs) acts as the primary transforming protein. E7 competes for retinoblastoma protein (pRb) binding, freeing the transcription factor E2F to transactivate its targets, thus pushing the cell cycle forwards. All HPV can induce transient proliferation, but only 16 and 18 can immortalise cell intes (in vitro).
It has also been shown that HPV 16 and 18 cannot immortalise primary rat cells alone; there needs to be activation of the ras oncogene. In the upper layers of the host epithelium, the late genes L1 and L2 are transcribed/translated and serve as structural proteins which encapsidate (Encapsidation is the process of incorporating a nucleic acid sequence (e.g., a vector, or a viral genome) into a viral particle) the amplified viral genomes.
Once the genome is encapsidated, the capsid appears to undergo a redox-dependent assembly/maturation event which is tied to a natural redox gradient that spans both suprabasal and cornified epithelial tissue layers. This assembly/maturation event stabilizes virions, and increases their specific infectivity.
Virions can then be sloughed off in the dead squames of the host epithelium and the viral lifecycle continues.
Latency period
Once an HPV viron invades a cell, an active infection occurs, and the virus can be transmitted. Several months to years may elapse before squamous intraepithelial lesions (SIL) develop and can be clinically detected. The time from active infection to clinically detectable disease makes it difficult for someone who has become infected to establish which partner was the source of infection.
Clinical Manifesations
Most people with genital HPV do not develop symptoms or health problems from it. In 90% of cases, the body’s immune system clears HPV naturally within two years. But there is no way to know which people who get HPV will go on to develop cancer or other health problems.
Sometimes, certain types of HPV can cause genital warts in males and females. Rarely, these types can also cause warts in the throat -- a condition called recurrent respiratory papillomatosis or RRP.
Other HPV types can cause normal cells in the body to turn abnormal, and might lead to cancer over time. These HPV types can cause cervical cancer and other, less common cancers, including cancers of the vulva, vagina, penis, anus, and head and neck (tongue, tonsils and throat). The types of HPV that can cause genital warts are not the same as the types that can cause cancer.
Diagnosis
Pap tests, looking for koliocytotic cells
PCR may be done on cervical swab.
no culture/serology
Treatment
Genital warts
Burning with liquid nitrogen
Immiquimod is an immune modulator. It is, however, expensive.
Podophyllin is cytotoxic; contraindicated in pregnancy.
The vaccine is helpful for preventing some subtypes of HPV (especially 6, 11)
Gardasil is a vaccine against HPV-16, -18, and two others.
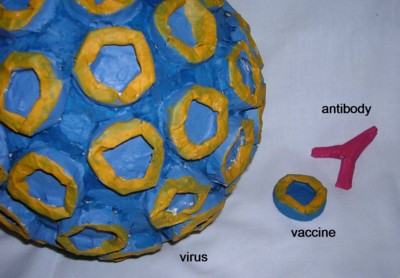
models created by Marissa LaPierre, 2007
Skin Warts
OTC are 18-27%.
40% salicycilic acid, cover with vaseline, and occulde with duct tape.
Cryotherapy
Liquid nitrogen is -196 C.
Can also use lasers, podophyllotoxin or omoquimod 5% cream for genital warts.
