
Malaria
last authored:
last reviewed:
recommended external resources
Introduction
(note: references required here)
Malaria is a serious disease caused by a parasite carried by certain types of mosquitoes. Humans are infected when bitten by the mosquitoes. Each year, there are 300 million to 500 million cases of malaria throughout the world and about 1 million child deaths. Every 30 seconds a child dies of malaria.
90% of all malaria deaths occur in sub-Saharan Africa and is responsible for a 1.3% growth penalty per year in some countries, due to loss in productivity (more than $12 billion in lost GDP every year).
In Africa, Malaria is the largest contributor to child morbidity for children under 5 years. It accounts for one in five of all childhood deaths in the continent. Malaria in pregnant women can lead to low birth weight, anemia and a greater risk of death to their newborn babies.
Epidemiology
Malaria is one of the world's most prevalent infectious diseases, with between 1-5 billion febrile episodes and 1-3 million deaths yearly, the majority occurring in sub-Saharan Africa (ref). Malaria is also common in Asia and South America.
Malaria has been recognized since the very earliest medical writing in China, India, and Assyria, where malaria-like intermittent fevers were attributed to evil spirits.
While endemic malaria is virtually non-existent in North America and Europe, Plasmodium should be considered in all travelers with fever.
However, Anopheles mosquitoes are found in North America. People infected with Plasmodium do have the capacity to lead to a re-development of endemic areas by being bitten by these mosquitoes.
Maps and descriptions of worldwide malaria can be found here:
The Plasmodium parasite
There are four species of parasite which commonly infect humans.
Plasmodium falciparum can cause high mortality rates and is associated with high levels of parasitemia. Daily fever often occurs.
P. vivax and P. malariae can cause relapsing disease long after primary infection because of latent infection outside erythrocytes, but symptoms are milder.
Gametocytogenesis requires approximately 10 days, and mosquitoes remain infectious for up to 4 days.
Transmission and Infection
Malaria is largely a blood-borne infection transmitted by Anopholes mosquitoes. Infection can also occur through blood transfusion or shared needles, leading to 'induced' malaria. Transplacental infection leading to congenital malaria is quite rare.
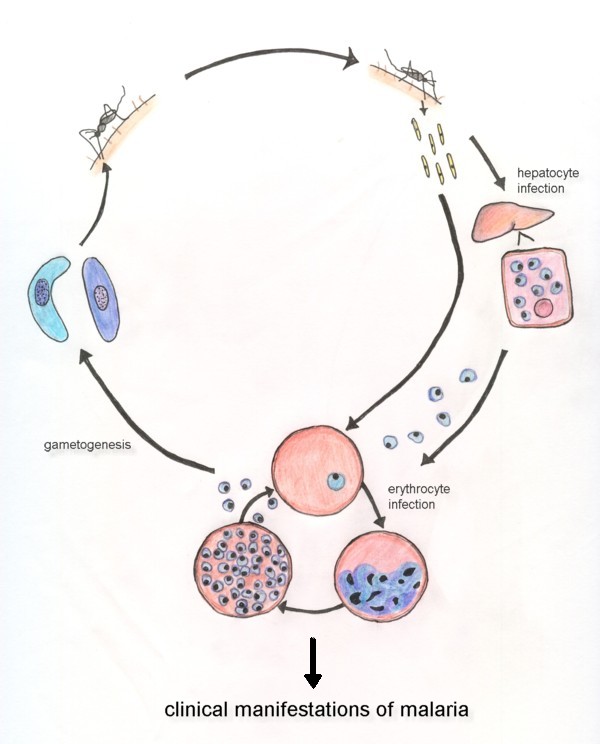
Sporozoites enter the blood stream via mosquito saliva, transit to the liver, and infect hepatocytes within 10-30 minutes. There, they proliferate and mature over 5-7 days, forming up to 40,000 merozoites before lysing the hepatocyte. Merozoites enter red blood cells within seconds.
Once inside a host RBC, merozoites divide asexually to form a schizont, composed of many (perhaps 20) merozoites. Erythrocytes undergo rapid and marked deformation as RBCs become less flexible and develop characteristic knobs on their surface, leading them to adhere to capillary walls.
Within 48-72 hours, infected RBCs burst, releasing many merozoites which then go on to infect other red blood cells.
Some merozoites develop into male or female gametocytes instead of proliferating. These gametocytes are taken up by mosquitoes and lead to sexual reproduction inside the mosquito's gut.
Signs and Symptoms
Symptoms tend to appear within 10-15 days of infection, though delays of several months are common.
During the first few days, fevers may be intermittent or low grade. As the disease progresses, fevers classically reach up to 41 C and last 6 hours, and are accompanied by chills, sweating, malaise, myalgia, and headache, nausea, and abdominal pain.
The asexual cycle is typically synchronous and periodic, leading to tertian or quartan fever cycles. P. Falciprum, vivax, and ovale malaria characteristically producess episodic fevers every 48 hours. P. malariae malaria requires 72 hours to complete the cycle. However, periodic symptoms are not invariable, and concomitant infections can lead to overlaping periods. Severe falciprum infection can cause continous fever.
As trophozoites mature, they become sequestered in capillaries of the brain, spleen, heart, skeletal muscles, and placenta.
Cerebral malaria is the most significant effect of falciprum infection.
Splenomegaly can result, and the liver, GI tract, and kidneys can all be affected. Hemoglobinuria, or blackwater fever, can result from accumulation of hemoglobin in kidney tubules.
Anemia results from both RBC rupture and bone marriw depression.
Falciprum malaria does not relapse - erythrocytes do not become infected from persistent liver infection once drugs or the immune system clear the blood. However, recrudescences - reinfection of RBCs by parasites in the blood - can recure for about 2 years.
Diagnosis
external resources:
Microscopy
Giemsa stain done on blood film is a useful diagnostic tool in expert hands. Identification is usually based in the presence of small ring-stage parasites, with multiple infections beinf common. Sequestration of trophozoites in capillaries means tghey are not normally visible in the peripheral circulation; their presence suggests severe disease.
Both thin and thick smears should be examined. When malaria is suspected and initial smears are limited, new blood should be examined at 6-hour intervals.
Rapid Diagnostic Testing
RDTs are fast, point-of-care methods of detecting malarial parasites in the blood. They are useful where microscopy-based diagnosis is unreliable or impossible. These kits require a cool storage conditions
Erythrocytes are lysed, and parasites are captured using antibodies.
A new technology involves optic detection of parasite-produced hemozin. (Biophysical Journal publication, 2008)
Serologic evidence of infection is useful for demonstrating past infection, but do not detect antibodies during ealy phases of acute infections. ELISA testing of sporozoite antigens can determine vector mosquito infection.
PCR testing facilitates rapid diagnosis and identification of malarial species, along with demonstration of drug sensitivity or resistance.
Preventing Malaria
Bed nets are one of the key methods of preventing infection.
Malaria is an environmental and sanitation issue, therefore, its spread can be mitigated through prevention and reduction of mosquito larva control, and promotion of clean and healthy environmental services. One way of reducing malaria infection is through reducing the breeding of mosquitoes.
There are different ways of reducing the breeding of mosquitoes e.g. habitat modification by draining stagnant waters that can be found in empty cans, bottles, gutters, broken vehicles, pot holes, and other water deposits; using chemicals e.g. pesticides; using natural predators e.g. larvae eating fish; and/or trapping larvae or adult mosquitoes.
Treatment
external articles:
Vaccine against gametocytes might work to prevent transmission, but will not prevent infection by sporozoites.
A malaria vaccine appears to be efficacious in children (Agnandji et al, 2011).
Recommendations for malarial prophylaxis and treatment are in a constant state of flux and depend on region.
Resources and References
Agnandji ST et al. 2011. First results of phase 3 trial of RTS,S/AS01 malaria vaccine in African children. N Engl J Med. 365(20):1863-75.
Roll Back Malaria, President’s Malaria Initiative, The World Health Organization, and Centers for Disease Control and Prevention
UNICEF; Water, Sanitation and Health
International Federation of Red Cross and Red Crescent Societies:
