
Staphylococcus aureus
last authored: Feb 2010, David LaPierre
last reviewed:
Introduction
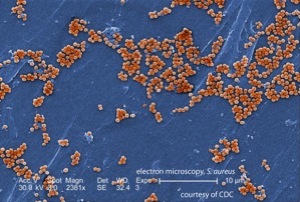
Staph aureus, courtesy of the CDC PHIL
Staphylococcus aureus is one of the most common and important pathogens, causing a variety of infections. S. aureus are large, gram positive cocci related to other Staphylococci, such as S. epidermiditis, S. saphyrophiticus, and S. lugdenensis.
The numerous virulence factors, exotoxins, and enzymes allow S. aureus to persist in humans and cause their many diseases. Many of S. aureus' virulence factors act locally to withstand phagocytosis and systemically to interfere with immune function.
The Case of Beth Swain
Beth Swain is a 35 year-old woman who develops a large, painful swelling on her leg after cutting it while in the woods one week ago. She notices pus draining from it. It worsens, and two days later she feels very unwell, with a high fever.
What is happening to Beth?
Epidemiology
People are frequently colonized by S. aureus, which is found in the nares of 10-20% of people. The bacteria may also transiently be found on the skin, oropharynx, vagina, and in the gut.
Incidence increases in hospitals, and it is the most frequent cause of nosocomial infections. They are very hardy, surviving for extended periods in dry conditions and proving difficult to eliminate from the environment.
Some people are more likely to be carriers, including health care professionals and people with diabetes, on hemodialysis, or IV drug users.
Classification and Characteristics
S. aureus is a gram positive cocci that grow in clusters (grapes). It is facultatively anaerobic.
CA-MRSA
- several clonal groups; PVL positive
Staph can grow on the skin and mucuous membranes in part due to MSCRAMMs which bind to extracellular matrix proteins.
Virulence Factors
peptidoglycan layer
Protein A
coagulase (aka clumping factor)
hyaluronidase
catalase
beta-lactamase
penicillin-binding protein 2a (PBP2a)
|
enterotoxins
hemolysins (alpha, gamma, delta toxins)
leukocidin
exfoliative toxins A and B
toxic shock toxin
|
Transmission and Infection
Infants may be innoculated with S. aureus shortly after birth, or it may be picked up throughout life. Some people will be long term carriers, while others are only intermittently colonized. Staph is transmissible person-to-person through direct contact or droplets.
Most infections are endogenous. S aureus does not normally penetrate tissues deeply except through burns, lacerations, bites, or surgical wounds.
Proliferation depends on number of organisms, site involved, and immune status. Bacteremia can follow skin infection and lead to seeding of highly vascular organs such as bone, joints, lungs, and kidney. There they can form other abscesses.
Clinical Manifesations
S aureus can cause some of the most varied disease manifestations of all bacteria. These include:
skin infectionsfolliculitis: small abscesses at the base of hair follicles
furuncles (boils): large, painful abscesses caused by deep inflammation of hair follicules and surrounding tissues
carbuncle: furuncles involving multiple adjacent follicles which coalesce to extend into subcutaneous tissue. Systemic symptoms are common.
cellulitis: diffuse involvement of subcutaneous tissue
impetigo: Usually involves exposed skin, particularly that of face and hands. Initial macules become multiple small pustules. Breaking pustules form shallow erosions covered with characteristic honey-coloured crusting serum. Highly infectious.
Lytic enzyme from Staph (alone or together with strep) cleaves desmoglein-1, a cell-cell adhesion protein, resulting in vesicle formation. bullous impetigo is a localized form of SSSS.
staphyloccal scalded skin syndrome: begins with peri-oral erythema that covers body within two days; large blisters are followed by desquamation but with no scarring. Toxin (exfoliatin A) related - from bacteria elsewhere
secondary skin infections: primary condition, ie atopic and diaper dermatitis, becomes infected, when protective epidermal barrier is broken
|
other infectionstoxic shock syndrome: due to systemic toxin superantigen; most commonly from respiratory or vaginal infection. Leads to fever, rash, and hypotension. Fatality rate is ~5%
food poisoning: due to enterotoxins; acute onset 2-4 h after ingestion; self-limiting after 12-24 hours
osteomyelitis
endocarditis, especially in IV drug users
bacteremia (one of the most common causes) with possible multi-organ seeding
CA-MRSAcauses serious community-acquired soft tissue or necrotizing infections
|
Diagnosis
Diagnosis is straightfoward. Abscess and/or blood should be aspirated, gram stained, and cultured.
Colonies are usually golden (giving the name aureus) but they may also be white.
Coagulase-negative Staph are distingished from S. aureus by the absence of coagulase production. The exception is S. lugdenensis, which produces sufficient clumping factor to be positive on a slide but negative in a tube.
Treatment
Almost all S. aureus produces beta-lactamase, and therefore most penicillins will not work against it. Cloxacillin is an exception and is standard treatment for methicillin-sensitive Staph aureus (MSSA). Second-line antibiotics include aminoglycosides, macrolides, TMP-SMX, clindamycin, and tetracyclines.
MRSA is resistant to all beta-lactams and is usually multi-drug resistant. Vancomycin is often used.
Community-acquired MRSA is generally susceptible to TMP/SMX, doxycycline, and clindamycin.
Clindamycin is particularly helpful due to its ability to prevent exotoxin synthesis, preventing systemic manifestations.
A handful of cases of vancomycin-resistant Staph aureus (VRSA) have begun emerging. Agents such as linezolid and daptomycin are effective, but represent the last line against an increasingly powerful bacteria.
