
Mycobacterium tuberculosis
last authored: March 2010, David LaPierre
last reviewed: Aug 2011, John Bwanika
Introduction
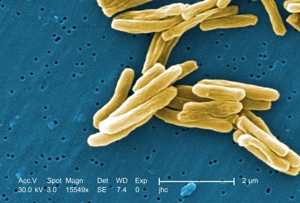
M. tuberculosis. scanning electron microscope
courtesy of CDC, PHIL #9997
Tuberculosis (TB) is a serious, yet curable chronic infection caused by the bacterium Mycobacterium tuberculosis (M. tuberculosis).
It affects healthy people, but can be devestating for the immunocompromised.
TB primarily affects the lungs, but can affect almost all other organs in the body. This can be as the primary focus of TB infection or as a secondary site following spread from the lungs.
Cases
Case 1
Ekanath Stanley is a 26 year-old man who applies to college to become a paramedic. As a part of his application he receives a TB skin test, which turns out to be positive.
- Does Ekanath have tuberculosis?
Case 2
You are running an outpatient HIV care clinic and a 33 year old man comes to your clinic with 1 month history of cough, on and off fever, drenching night sweats and also reports to have 10kgs of weight over the past 2 months.
- What differential diagnoses will you have for this patient?
- How will you go on to investigate this patient and arrive at the final diagnosis?
Case 3
James is a 30 year old man who comes to you in an outreach HIV clinic in a rural district of Uganda. He is wasted and he has multiple swellings in the neck and inguinal area.
He reports that over the 3 months that he's had those swellings, he has had low grade fever, night sweating and has also lost a considerable amount of weight. He was tested for HIV 6 months ago and found to be HIV seropositive but he is not under any care because he cannot access any in his district.
- What differential diagnoses would you have for James?
- What treatments may be offered to him?
Epidemiology
Worldwide, 1/3 of the world's population is infected with TB, and over 16 million existing cases of disease and 8 million new cases occur each year. It is an important complication in patients with AIDS and is one of the leading causes of death among HIV patients.
Countries with the highest TB prevalence are found in Southeast Asia, sub-Saharan Africa, and Eastern Europe, although resurgence is occurring in many developed countries.
These also happen to be countries with high prevalence of HIV and low socio-economic status with poor housing and accommodation facilities.
Risk factors predisposing people to TB exposure include:
- being born in a high-risk country (Cain et al, 2008)
- travelling to countries with high prevalence
- Native American populations in North American cities
- homeless, poor, malnourished, elderly
- prisoners
- intravenous drug use
- Sharing poor and crowded accommodation facilities with a TB patient especially those with smear positive open lung cavities.
Risk factors for developing active TB include:
- immunosuppressed individuals like HIV patients or transplant patients
- other active lung disease, ie mixed dust pneumonoconeosis
- recent TB seroconversion
Classification and Characteristics
M. tuberculosis is a slightly curved or straight bacilli. It is aerobic, non-motile, and slow-growing (doubling time 18h).
The bacterium is known as acid-fast due to high concentration of mycolic acids (lipid) in cell wall that withstands decolorization by alcohol during Ziel-Nielsen staining.
Most strains grow on relatively simple media (Lowenstein-Jensen media); some are fastidiuous and some cannot be cultured.
M. tuberculosis lives in intracellular vesicles within macrophages, inhibiting lysosomal merging.
Transmission and Infection
uberculosis can be transmitted in five ways:
- inhalation (most common)
- ingestion
- through breaks in skin (rare)
- intercourse (rare)
- intra-partum (rare)
Inhalation of airborne droplets (nuclei) 1-5 μm in size results in deposition in the lungs. Higher oxygen tension in the upper lobes facilitates bacterial growth. Probability of transmission includes infectousness of person, environment and duration of exposure, and virulence of organism. A 50% infective dose is <10 bacilli.
Once settled in the terminal airways, bacteria are phagocytosed by unactivated alveolar macrophages. Phagosomal acidification and lysosomal fusion are prevented, and the bacteria multiply freely. Infected macrophages eventually are destroyed, with further cycles of phagocytosis, bacterial proliferation, and lysis occurring.
Presentation of bacteria bits on MHC II molecules activates a CD4+ Th1 response, resulting in IFN-gamma production and angry macrophage transformation. This attenuates bacterial activity.
Circulating macrophages and lymphocytes are attracted to the area of infection, forming multinucleated giant cells formed from fused macrophages (Langerhans cells) and resulting in granulomas.
Clinical Manifesations
Tuberculosis has three stages: primary, latent, and post-primary (secondary).
Primary Infection
Primary infection is asymptomatic, though symptoms can be seen in children and HIV+ adults. Macrophages ingest the bacterium, which survive and multiply. Infected macrophages travel to local lymph nodes forming the Ghon complex, as well as into the blood stream and to other tissues such as bone marrow, spleen, kidneys, and the CNS. There, small granulomas form with epitheliod and giant cells present.
Granulomas can have cheesy, necrotic insides (caseation when small or cavitation when larger).
Latent Tuberculous Infection
LTBI follows a primary infection. Over a lifetime, 10% of people will progress to develop active disease.
Active Disease
Pulmonary TB often appears as chronic productive cough, with or without hemoptysis. Sputum may be scanty, purulent, or bloody. Sputum and hemoptysis suggests tissue destruction or invasion of blood vessel, as accompanies cavitary disease. One or both upper lobes are usually involved in patients with active disease, resulting in pneumonitis, absecess formation, or cavitation. Chest X-ray can show consolidation, cavitation, and lymphadenopathy.
Miliary TB represents widely spread bacteria, with seeding across the lungs, abdomen, bone marrow and CNS. It derives its name from the seed-like (millet) appearance of multiple 2-4 mm lesions, as can be seen on X-ray. It can commonly be seen among patients with severe immune suppression as those with late stage HIV and not on HAART.
Extrapulmonary TB can have many manifestations, including lymphadenitis, pericarditis, pleuritis, hepatitis, peritonitis, meningitis, osteomyelitis (Pott's disease of the vertebra), adrenal infection (Addison's disease), pyelonephritis, ovary infection and less commonly the skin.
Secondary TB is reactivation of bacteria. Clinical manifestations are primarily due to host response to infection, and the enhanced immune response causes significant damage. They develop slowly and are nonspecific, including
- malaise
- fever
- anorexia and weight loss
- night sweats
As CD4+ cells die as is commonly the case among HIV patients, latent TB infections can emerge from macrophages, become reinfectious, and spread around the body.
TB Skin Testing
In the younger patients, the goal of TST is to identify patients with latent TB, and to determine needs for prophylaxis. For older patients, the test is more used to identify active TB. Unfortunately, it is negative in 25% of patients with active TB.
Targets for screening should include:
- contacts of an active case
- foreign-born patients <20, arrived in the last two years
- refugees, up to 50, from high incidence countries
- other adult immigrants with risk factors
- X ray evidence of old, active TB, with no history of treatment
- patients with a high risk of progression to active disease (eg immunocompromised patients; receiving medication for RA, Crohn's, HIV, diabetes)
- health care providers
- staff and residents in long term care, corrections, or homless facilities
Contraindicications include:
- documented past history of active TB, treatment for LTBI, or documented TST >10mm
- blistering TST reaction
- current major acute viral infection (eg measles)
- live vaccines within past few weeks (eg MMR)
Contraindications are NOT:
- had a BCG
- undocumented 'positive' TST without blistering
- colds
- low-dose steroids
- pregnancy and breastfeeding
Interpreting the TST
Size of the reaction
Positive predictive value
Risk of progression from latent to active disease
TST
|
consider positive in: |
0-4 mm |
children |
>5 mm |
|
> 10 mm |
An online TST calculator can be seen here - www.tstin3d.com
False positive tests can be seen with:
- BCG (especially with immunization after 1 year)
False negative tests can be seen with:
Diagnosis

courtesy of CDC, PHIL #6806
The PPD (Mantoux) test uses delayed type hypersensitivity to diagnose the presence of CD4+ Th1 memory cells, suggesting prior or current infection. False negative tests occur in 20-25% of people, and BCG vaccinations can result in a high level of false positives. Conversely, overwhelming TB can cause the Mantoux test to be negative.
In countries of high TB burden and wide spread infant vaccination with BCG, the mantoux test is highly unreliable and further investigations are needed to confirm the diagnosis of TB.
If the TST is in question, an IGRA is an acceptable.
Active TB should be diagnosed with further imaging, eg CXR and/or CT. Serial sputums should be done
Chest X rays of TB, courtesy of Dr John Bwanika

left upper lobe cavitation

miliary TB

left pleural effusion
Typical physical exam will reveal a wasted patient, low grade fever, who may or may not have lung crepitations, features of consolidation or effusion.
Other physical presentations will depend on the type of tuberculosis and it's focus.
Chest X ray and physical examination can result in findings of consolidation or cavitation in the apices of the lungs.
Ultimately, tuburcle bacilli must be identified although this may not be an easy task among severely immunocompromised patients and those with extra-pulmonary tuberculosis.
Acid-fast smears or auramine-o fluorescent staining of sputum should be performed. Liquid media culture can provide results within two weeks, while conventional cultures can take up to 10 weeks. Culture remains the gold standard, as it allows drug resistance testing.
Urinalysis classically reveals sterile pyuria. Early morning samples are best.
PCR amplification can detect as few as 10 bacteria, as compared to 10,000 required for smear diagnosis. Rapid molecular testing can identify drug-resistant TB with high accuracy (Boeme et al, 2010).
Histology
Pathologic features include:
- Ghon focus: parenchymal nodules
- Ranke's complex: Ghon focus associated with an enlarged hilar lymph node
- Necrotizing granulomas are often present (though also associated with other infections as well)
Treatment
Isolation practices are required for patients with active TB, which demonstrates airborne spread.
Anti-mycobacterial agents are used in combination, and treatment usually takes 2 phases. Fuller details regarding medical treatment of TB are described here.
Prevention
BCG vaccine is used in areas where TB is prevalent.
Resources and References
http://www.coregroup.org/storage/TB/Community-Based_TB.pdf
Canadian Tuberculosis Standards
Greenaway et al. 2011. Tuberculosis: evdience review for newly arriving immigrants and refugees. 183(12):E...
Boeme CC et al. Rapid molecular detection of tuberculosis and rifampin resistance. N Engl J Med. 363(11):1005-15.
Cain KP et al. 2008. Tuberculosis Among Foreign-Born Persons in the United States. JAMA. 300(4):405-412.
Sterling TR et al. 2011. Three months of rifapentine and isoniazid for latent tuberculosis infection. N Engl J Med. 365(23):2155-66.
