
Shoulder Dystocia
last authored: July 2010, David LaPierre
last reviewed: Nov 2010, Dr Zeke Milklovic
Introduction
Shoulder dystocia is the inability to deliver an infant's shoulders after the head is delivered, resulting in a serious obstetric emergency. All health care providers involved in labour and delivery should be prepared for this possibility, which occurs in 1:200 - 1:400 deliveries, or over 1:75 deliveries if the fetus is >4000g.
The Case of Florence A.
Florence is a 16 year-old women pregnant with her first child. She has not been followed by a health care provider during her pregnancy. She presents to the regional hospital in labour. After 30 hours of labour, the head delivers and then stops.
- What should the delivering doctor do?
- What are the potential consequences of this situation?
Causes and Risk Factors
Over 50% of cases of shoulder dystocia are unexpected. However, established risk factors include:
- maternal diabetes (principal risk factor)
- post-term pregnancy
- fetal macrosomia
- induction
- prolonged labour, especially in second stage
- operative vaginal delivery, especially midforceps delivery
- previous shoulder dystocia
- older mother
- grand multiparity (five deliveries or more)
Pathophysiology
Shoulder dystocia occurs when the anterior shoulder becomes stuck on the pubic symphysis, or when the posterior shoulder hits the sacral promontory.
Signs and Symptoms
- history
- physical exam
History
All mothers should be screened for risk factors, as described above. This should prompt discussion of elective C-section or transfer of care before labour to a centre offering C-section.
Physical Exam
Leopold's maneuvers may be helpful to predict macrosomia.
Diagnosis is made when the infant does not deliver past the head. The 'turtle sign' occurs when the head recoils against the perineum.
Investigations
No investigations are warranted once shoulder dystocia occurs. It may be predicted, however, with impaired fasting glucose or ultrasound revealing macrosomia.
Differential Diagnosis
Abdominal dystocia, when the abdomen of the infant becomes wedged in the birth canal, is rare.
Management
note: this section will benefit from two illustrations similar to those in this article
If you are involved in labour and delivery, always be prepared, mentally and with equipment, for the possibility of shoulder dystocia.
Patients should be informed of the risk of shoulder dystocia if the fetus is estimated to be over 5000 grams, or if over 4500 grams in a mother with diabetes, and discussion of elective cesarian section should be discussed. Elective C section should not be standard, as the the number of C sections needed to prevent one brachial plexus injury is nearly 3,700. However, in patients at high risk for shoulder dystocia, it may be reasonable to transfer the patient with C-Section capabilities.
Newest research supports a two-step approach to delivering the baby: waiting for the head to fully restitute and then using maternal pushing efforts during the next contraction. It is now evident that waiting for up to four minutes between contractions is common and safe and reduces the risk of shoulder dystocia while maintaining normal cord gases. If after the next contraction the baby is not delivered despite maternal pushing efforts, a shoulder dystocia should be diagnosed and managed as seen below. (Kotaska and Campbell, 2014).
ALARMER - Acronym for actions to address shoulder dystocia
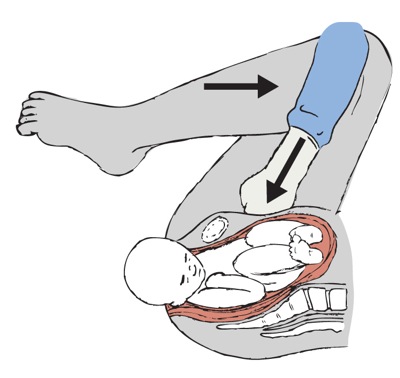
the L and A from ALARMER - illustration by Alison Martin
Ask for help: ask patient to push hard, ask nursing to drop head of bed down, and call for anesthesia and the pediatrician.
Legs: hyperflex legs (McRobert's manoeuvre) to open pelvis in AP direction (helpful in up to 40% of shoulder dystocias).
A: Disimpact the Anterior shoulder with suprapubic pressure (not fundal presure); push against the posterior shoulder. You can also attempt to rotate shoulders to oblique plane by inserting two fingers posteriorly into the vagina and pushing on the front posterior shoulder to move it off the midline
Release posterior arm: find fetal forearm and hand and sweep it across the chest
Maneuver of Woods - Corkscrew maneuver
Episiotomy: not helpful to free infant, but can create more room
R: roll mother onto all fours to free impacted shoulder.
Avoid fundal pressure or excessive traction/twisting of the infant neck, as these maneuvers cause more harm than good.
Other rare options include:
- deliberate clavicle fracture
- Zavenelli maneuver - push baby back inside and do C-section
- symphysiotomy
Active management of the third stage is important; be prepared for postpartum hemorrhage. Examine the mother and infant for injury. Perform cord gases.
Thorough documentation and discussion with the patient after delivery is helpful for future medical care and potential legal challenges.
Consequences and Course
Most cases of shoulder dystocia resolve without complication. The most common fetal/neonatal complication is brachial plexus injury, although most (75-90%) resolve completely. Other complications include fractures (clavicle, humerus), asphyxia, and death.
Maternal complications can include (severe) genital tract lacerations, postpartum hemorrhage, rectovaginal fistula, symphyseal separation, uterine rupture, and psychological trauma.
Resources and References
Baxley EG and Gobbo RW. 2004. Shoulder Dystocia. American Family Physician. 69(7):1707-1714.
Kotaska A, Cambell K. 2014. Two-Step Delivery May Avoid Shoulder Dystocia: Head-to-Body Delivery Interval Is Less Important Than We Think. Journal of Obstetrics and Gynaecology of Canada. 716-720.
Topic Development
authors: David LaPierre, 2010
reviewers: Dr Zeke Milkovic, Nov 2010
