
Placenta Previa
last authored: June 2009, Reuben Kiggundu
last reviewed: April 2010, James Andrews, MD
Introduction
Placenta previa is the presence of placental tissue lying over the cervical canal or right next to it. It complicates 1:250 term pregnancies (over 37 weeks)
Placenta previa occurs when the embryo implants in the lower part of the uterus, near the cervix. This is a very serious and potentially life-threatening situation. As the pregnancy advances and the uterus grows, the lower segment of the uterus will stretch and thin out. This may cause some of the placental blood vessels implanted in this area to spontaneously tear or rupture and may result is significant painless vaginal bleeding. With placenta previa, the placenta is located lower than the developing fetus and obstructs the cervical canal. The only safe option for delivery in this situation is a cesarean section.
Alison Martin, 2010
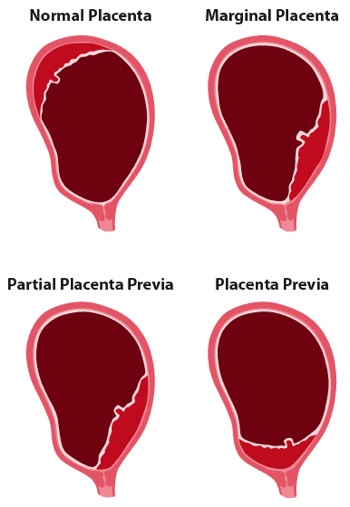
There are various classification schemes for placenta previa. Traditionally, placenta previa's were classified as marginal, partial or complete, in increasing order of severity:
marginal: placental edge near the cervical os
partial: placental edge next to the cervical os
complete/central: placenta completely
covers the cervical os
With the use of ultrasound in obstetrics today, a more contemporary classification scheme is used:
marginal placenta previa: placental edge lies within 2 cm of the cervical os but does not cover it
placental previa: placenta completely covers the cervical os
The Case of Mary Bankole
Mary Solarin is a 34 year-old woman living in rural Kenya, 32 weeks pregnant with her third child. Her pregnancy has progressed uneventfully, and she has seen no one other than the village community health worker. She awakes to find her bedsheets soaked with blood. She is experiencing no contractions. Her husband rushes her to the nearest hospital, 30 km away, by public transit.
- What should the emergency room doctor evaluate?
- What should initial treatments be?
- What are possible outcomes for her pregnancy?
Causes and Risk Factors
Risk factors for placenta previa include:
- multiparity
- previous history of placenta previa
- increasing maternal age
- previous uterine curettage
- previous cesarean section
- previous uterine surgery
- chronic hypertension
- smoking
- multiple gestation
- cocaine use
Pathophysiology
Placenta previa is initiated by implantation of the embryo in the
lower segment of the uterus. As the placenta develops and grows,
it covers the internal cervical os.
Bleeding is thought to occur secondary to the thinning of the lower
uterine segment which is a normal ongoing process as the uterus
enlarges and stretches throughout pregnancy. The placental
attachments in the lower segment may tear during this process or with
cervical dilatation. Bleeding is typically painless, bright red
and unpredictable with most episodes occurring spontaneously without
any preceding event.
Most women today have a second trimester ultrasound to review fetal
anatomy and for placental location. Consequently, most women are
diagnosed with a placenta previa before they develop vaginal bleeding
and are therefore aware and educated about their diagnosis before
problems arise. If a patient is noted to have a placenta previa
or low-lying placenta on their routine second-trimester ultrasound,
they should be rescheduled for a follow-up scan in the third trimester
for repeat placental localization. In many women with a marginal
placenta or placenta previa diagnosed in the second trimester, the
placenta will have 'migrated' far enough away from the cervix by term
to allow for safe vaginal delivery. It should be noted that the
placenta itself does not move throughout pregnancy, however the growth
and stretching of the lower segment effectively shifts the placenta
away from the cervical canal. Vaginal delivery can be attempted
in women with a low-lying placent if the edge is more than 2-3 cm away
from the internal cervical os.
Signs and Symptoms
- history
- physical exam
History
Painless bright red bleeding in the third trimester. Bleeding may be severe and cause symptoms of shock.
Physical Exam
Vaginal/Cervical examination is contraindicated in patients who present with third-trimester painless vaginal bleeding until a placenta previa can be ruled out by ultrasound. A digital cervical exam in a patient with a placenta previa can result in a catastrophic hemorrhage if the examining fingers tear the placenta during the examination.
Therefore, before examining a patient with vaginal bleeding in pregnancy their chart should be reviewed to identify the location of the placenta if they have had a previous ultrasound.
Investigations
- lab investigations
- diagnostic imaging
Lab Investigations
- CBC - to look for maternal anemia
- Kleihauer-Betke test - can be helpful to determine if fetal-maternal hemorrhage has occurred (detects fetal red blood cells in the maternal circulation)
- Maternal Blood Type and Antibody screen - if Rh negative, will
need Rh immune globulin
- APTT,PT, Fibrin degradation products - to rule out DIC (disseminated intravascular coagulation - rare with previa but may occur with massive hemorrhage)
Diagnostic Imaging
Transabdominal ultrasound will identify 95% of cases of placenta previa. Transvaginal ultrasound has a diagnostic accuracy of almost 100% and is safe in patients with a placenta previa when performed by an experienced sonographer.
Differential Diagnosis
The differential diagnosis for antepartum bleeding in the third-trimester includes:
- placenta previa
- placental abruption
- vasa previa
- uterine rupture
- cervicitis, cervical polyp, cervical ectropion, cervical cancer
- preterm labor (bloody show)
- premature rupture of the membranes
- intercourse
- vulvovaginitis
Treatments
Management when diagnosed at routine second-trimester ultrasound and no bleeding:
- can be managed safely as an outpatient if compliant patient who
lives close to medical facilities
- counsel patient to avoid intercourse and digital cervical exams
- avoid strenuous exercise and decrease physical activity
- educate to seek medical attention if bleeding or uterine contractions develop
- follow-up third trimester ultrasound for placental location and fetal growth
If placental edge is greater than 2-3 cm away from the
internal cervical os, then vaginal delivery can be safely attempted.
Management if presents with antepartum hemorrhage:
- NPO
- Large bore IV access x 2 and volume replacement
- Lab work:
- CBC
- Blood type and screen
- X-match 4 units
- coagulation studies
- kleihauer-betke
- Maternal monitoring - vitals, urine output
- Fetal heart rate monitoring - continuous electronic fetal monitoring
- If Rh negative - will need Rh immune globulin (WinRHO, RhoGAM)
If bleeding stabilizes:
- admit to hospital for observation
- bed rest
- fetal growth ultrasound
- transfusion if necessary
- administer antenatal corticosteroids to promote fetal lung maturity if <34 week
Indications for immediate delivery by cesarean section:
- persistent abnormal fetal heart rate tracing
- life-threatening severe maternal hemorrhage
- unrelenting labour
- significant bleeding >34 weeks (fetus is reasonably mature)
Counsel patients with placenta previa about risk of recurrence and ask them to see an obstetrician early on during the next pregnancy.
Consequences and Course
Maternal Complications:
- Hemorrhage - anemia, need for blood transfusion, hypoxia and
end-organ damage from decreased perfusion
- Maternal mortality <1% in developed countries
- Surgical risks from cesarean section
- Placenta accreta (1-5%, higher if the patient has had a
previous c-section)
Fetal Complications:
- Intrauterine fetal demise (IUFD)
- Intrauterine growth restriction (IUGR)
- Preterm delivery ~50%: major cause of perinatal morbidity and mortality
Recurrence Risk in a subsequent pregnancy is between 4 and 8 percent.
Resources and References
Gabbe et al., Antepartum hemorrhage. Obstetrics: Normal and
problem pregnancies, 5th edition. Mosby 2007.
Topic Development
authors:
reviewers:
