
First Trimester Bleeding and Miscarriage
last authored: August 2010, Kim Colangelo
last reviewed: Feb 2011, Jessica McPherson
Introduction
A miscarriage, or spontaneous abortion, is a pregnancy loss at less than 20 weeks of gestational age or less than 500grams.

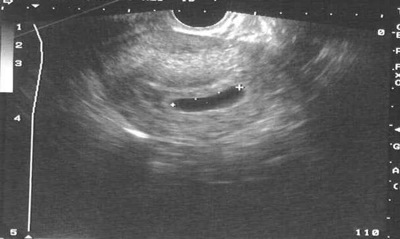
Missed abortion (courtesy of FMDRL)
A miscarriage at less than 6weeks from the last menstrual period is called an early pregnancy loss. A fetus is not usually viable before 24 weeks. Fetal demise beyond 20 is termed stillbirth.
The true incidence of spontaneous abortion is difficult to ascertain since not every woman with a spontaneous abortion will present to a health care professional, or even be aware of her condition. An early pregnancy loss may be mistaken for a heavy period, it may last slightly longer, have heavier bleeding, and/or clots or tissue may be passed. Most sources suggest that 10-15% of clinically recognized pregnancies end in spontaneous abortions.
A miscarriage is a broad term that can refer to an inevitable, incomplete, complete or missed abortion.
First-trimester bleeding is called a threatened abortion.
The Case of Ms. Li
Ms. Li is a 36yo G2T0P0A1L0 who presents to the emergency department at 9weeks gestational age with vaginal bleeding and suprapubic pain. She is extremely distressed because her last pregnancy ended in a loss at 11 weeks.
- What condition do you need to rule out?
- What is on your differential as a cause of the bleeding?
Causes and Risk Factors
Risk factors:
- Advanced maternal age
- Previous spontaneous abortions
- Smoking, possibly alcohol and cocaine
- Extremes of weight (under and over)
- Conception within 3-6months of a delivery
- Possibly NSAIDs (excluding acetaminophen)
- Possibly caffeine (likely more than 500mg/day)
- Possibly celiac disease that is untreated
Causes

by Corinne Ladd
It is not always possible to determine if the fetus/embryo was abnormal since some spontaneous abortions produce an empty gestational sac and sometimes what is present is unable to be examined.
- Chromosomal
- Trauma
- Congenital anomalies
- Structural abnormality that interferes with implantation such as uterine septum or adhesions
- Infections
- Autoimmune disease
Approximately half of all miscarriages are due to chromosomal abnormalities, often aneuploidies that are not compatible with fetal life. The most common is an autosomal trisomy followed by polyploidy (more than two sets of chromosomes), and then monosomy X.
Congenital anomalies have many causes; an example would be teratogens such as environmental exposures like lead or maternal medications such as chemotherapy drugs. There are certain autoimmune diseases that pose a high risk of miscarriage, often this is due to a hypercoagulable state resulting in compromised blood flow to the placenta. Two examples would be antiphospholipid antibody syndrome and systemic lupus erythematosus.
Examples of infections known to be associated with an increased risk of miscarriage are bacterial vaginosis, mycoplasma, herpes simplex virus, toxoplasmosis, listeriosis, chlamydia, human immunodeficiency virus, syphilis, parvovirus B19, malaria, gonorrhea, rubella, cytomegalovirus.
Pathophysiology
Approximately half of all miscarriages are due to chromosomal abnormalities, often aneuploidies that are not compatible with fetal life. The most common is an autosomal trisomy followed by polyploidy (more than two sets of chromosomes), and then monosomy X. Congenital anomalies have many causes; an example would be teratogens such as environmental exposures like lead or maternal medications such as chemotherapy drugs.
There are certain autoimmune diseases that pose a high risk of miscarriage, often this is due to a resulting hypercoagulable state resulting in compromised blood flow to the placenta. Two examples would be antiphospholipid antibody syndrome and systemic lupus erythematosus.
Examples of infections known to be associated with miscarriage are bacterial vaginosis, mycoplasmosis, herpes simplex virus, toxoplasmosis, listeriosis, chlamydia, human immunodeficiency virus, syphilis, parvovirus B19, malaria, gonorrhea, rubella, cytomegalovirus.
Signs and Symptoms
- history
- physical exam
History
When a pregnant woman presents with vaginal bleeding before twenty weeks, it is important to quantify the amount of blood lost. Questions to help with this can include asking if the patient is wearing a pad and how often it needs to be changed, and whether there is blood in the toilet bowl or only when she wipes after urination. Also ask about the color of blood and if clots or tissue are present. Always assess the hemodynamic stability so along with vital signs ask about dizziness or feeling faint, nausea or headaches. If there is recurrent pregnancy loss, >=3, ask about reproductive anomalies, autoimmune conditions in the woman or the family, thyroid problems, diabetes, smoking, alcohol, and recreational drug use.
In all types of spontaneous abortion except for complete abortions, a septic abortion, infection of the uterus and products of conception, is possible, usually by the retention of the fetal or embryonic tissue. As such, ask about fever, foul-smelling discharge, vaginal bleeding that does not stop, cramping and malaise. An infected/septic abortion may also occur as a consequence of organisms being introduced via procedures such as amniocentesis, foreign bodies such as IUDs or via an illegal induced abortion.
threatened |
inevitable |
incomplete |
complete |
missed |
|
Symptoms |
bleeding |
bleeding, cramping |
bleeding, cramping |
resolved bleeding and cramping |
resolution of pregnancy symptoms |
Passage of Tissue |
no |
no |
possibly |
finished |
no |
Cervix |
closed |
open |
open |
open, then closed |
closed |
Viability |
perhaps |
no |
no |
no |
no |
Physical Exam
When a patient presents with bleeding, it is difficult to assess the actual amount of blood loss by history alone so vitals including heart rate, blood pressure, respiratory rate, O2 saturation and temperature should be measured.
If there is no placenta previa, a vaginal exam may be performed to see if the cervix is open or closed. This is safe to do before 12 weeks gestational age without ultrasound.
Attempt to obtain a fetal heart by bedside Doppler, depending on the circumstance.
If there were no contractions and the cervical os is open, the woman may have an incompetent cervix. It can be difficult to distinguish from an inevitable abortion as both will have an open cervix. In an inevitable abortion the uterine contractions lead to the cervical os opening versus an incompetent cervix has the cervical os open without any contractions. An incompetent cervix can be treated.
Investigations
- lab investigations
- diagnostic imaging
Lab Investigations
In cases of first-trimester bleeding, lab investigations to be done should include:
- blood type and antibody screening to determine if Rh immune globulin, including WinRho and RhoGAM, is indicated (this is recommended by the Society of Obstetricians and Gynaecologists of Canada although there is no clear evidence for this during threatened abortion)
- CBC to verify hemoglobin, possible leukocytosis as a sign of infection and platelet count
- B-hCG levels can be followed, in which case they should be collected two or more times. A single value does not indicate a viable pregnancy and it does not indicate that a pregnancy is intrauterine or ectopic. A falling hCG may be due to a miscarriage or to a resolving ectopic. In a completed abortion, the hCG should halve every 48-72hrs until zero. If they do not attain zero, then there are retained products of conception. A rise of >66% is suggestive of normal intrauterine pregnancy, less than that suggests ectopic or abnormal pregnancy.
- A serum progesterone level may be drawn. Less than 25nmol/L is associated with non-viable pregnancies, however this is not a rule and treatment should not be based solely on a low progesterone level.
Diagnostic Imaging
Ultrasound can be used to confirm intrauterine pregnancy if that has not yet been done. U/S may also be used to assess viability (eg fetal heart rate), retroplacental bleeding, and retained products of conception.
It is important to rule out an ectopic pregnancy. This can be done by transvaginal ultrasound if the B-hCG level is above 1500-2000 mIU/mL.
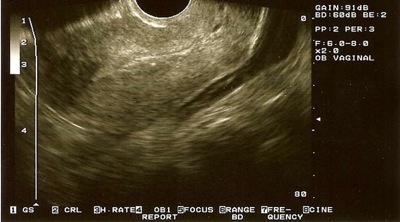
Anembryonic gestation seen as a gestational sac >18mm without a yolk sac or fetal pole, taken from Family Medicine Digital Resource Library, Office management of miscarriage, Creative Commons License)

Missed abortion seen as a fetus with no cardiac activity and a closed cervix, taken from Family Medicine Digital Resource Library, Office management of miscarriage, Creative Commons License)
Incomplete abortion seen as retained products of conception on ultrasound and a vaginal exam revealing an open cervix, taken from Family Medicine Digital Resource Library, Office management of miscarriage, Creative Commons License)
Differential Diagnosis of First Trimester Bleeding
- Physiologic, aka implantation bleed
- Miscarriage: including inevitable, incomplete, complete or missed abortion
- Inevitable abortion - bleeding associated with dilatation of the cervix
- Incomplete abortion - bleeding associated with passage of some, but not all, of the products of conception
- Complete abortion - the passage of all the products of conception from the uterus
- Missed abortion - the fetus or embryo has died, but no tissue has yet to pass through the cervix. We now know that this is the case for a period of time in the vast majority of all spontaneous abortions.
- Ectopic pregnancy
- Gynecological abnormality such as polyps, fibroids, neoplasm
- Incompetent cervix leading to miscarriage
- Molar pregnancy – vaginal bleeding, absence of fetal heart sounds, elevated hCG, snow storm on U/S
- Infection of the cervix/vagina
- Subchorionic hemorrhage
Treatments
If a patient presenting with bleeding appears to be hemodynamically unstable,
- call for help
- insert two large bore IV’s with fluids running
- order crossmatched blood
Unfortunately, for patients who are diagnosed with threatened abortion, continued research has failed to show evidence of any promising therapies. Recent reviews have not demonstrated a decreased rate of spontaneous abortion with:
- the administration of progestogen (Wahabi et al., 2011)
- anticoagulants (except in the case of hypercoagulability syndromes) (Kaandorp et al. 2009)
- bed-rest
- hCG (Devaseelan et al, 2010).
Though it may be difficult to distinguish from incomplete abortion, the open cervix associated with incompetent cervix is less likely to be accompanied by cramping or pain. In this case, cervical cerclage is performed to prevent loss of the pregnancy. This can be opened at term to allow for vaginal delivery, or maintained and C-section done.
If a spontaneous abortion is confirmed, the woman should be allowed to choose which treatment she they will follow where possible. Her options include:
Expectant management, which may take several weeks, can be an option for incomplete, inevitable and missed abortions in which there is no immediate danger of sepsis or hemorrhage. In about 50% of cases, the abortion will be completed within 7 days. Otherwise, she may elect to try a different treatment option.
Medical evacuation is usually attempted by misoprostol administration, which is a prostaglandin analogue. It is often given vaginally. If early in pregnancy, the abortion will complete within 7 days in approximately 85% of cases. Oxytocin may also sometimes be administered.
Surgical uterine evacuation via curettage or vacuum aspiration has nearly a 100% success rate in achieving completion of the abortion, though complications can include infection, bleeding, uterine perforation or Asherman syndrome. The complication rate is not significantly higher than that of medical management.
Consequences and Course
It can take anywhere from a few hours to a few days for a miscarriage to be complete.
Women often resume normal menstrual cycles in 1 month; they can become pregnant immediately however they may not be emotionally ready. The level of grief and distress is not necessarily related to how far along the pregnancy was, since the parents can bond with and be excited for the fetus at an early gestational age. It is common to experience depression, anxiety and guilt following a pregnancy loss. Postpartum support for both parents should be provided.
If there have been recurrent pregnancy losses, investigate to find the reason as guided by the history.
Additional Resources
www.nationalshare.org - a website for support for parents after a pregnancy or infant loss
Griebel, C., et al. Am Fam Physician. 2005 Oct 1;72(7):1243-1250.
References
Devaseelan et al., Cochrane Database Syst Rev. 2010 May 12;(5):CD007422
Kaandorp et al., Cochrane Database Syst Rev. 2009 Jan 21;(1):CD004734)
Wahabi et al., Cochrane Database Syst Rev. 2011 Mar 16;3:CD005943
Topic Development
authors: Kim Colangelo, July 2010
editors:
reviewers:
