
Placental Abruption
last authored: July 2010, Kim Colangelo
last reviewed: Dec 2011, Cheryl Renaud
Introduction
A placental abruption (abruptio placentae) is when a normally implanted placenta separates from the uterus after 20 weeks gestation (less then 20 weeks gestation is considered a spontaneous abortion). It occurs in approximately 0.5-1% of pregnancies in North America (Broers et al, 2004). The peak gestational age for placental abruption is 24-27weeks.
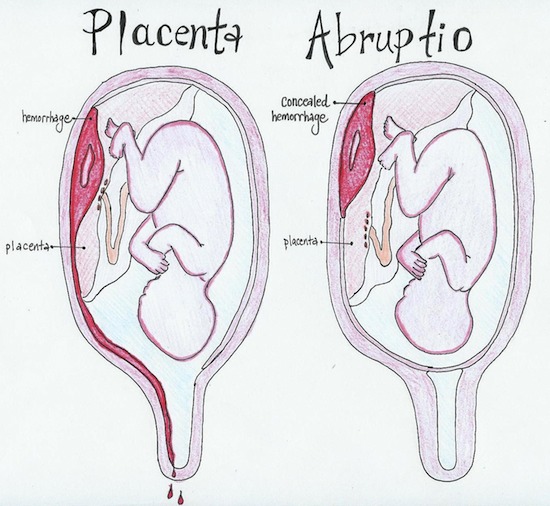
illustrated by Erin Chia
The abruption can be a total or a partial depending on how much of the placenta separates, and may be graded as can be graded as mild, moderate or severe.
The abruption can be external/revealed/apparent where blood flows out of the cervix, as shown on the left.
Conversely, it can also be internal/concealed, where blood remains in the uterus and is not seen outside the vagina.
The Case of Mrs Thomas
A 37yo G4P3 woman presents to the emergency department with vaginal bleeding. She is 32 weeks along with twins. She states that she was grocery shopping when she noticed it and came directly to the hospital. It has not subsided and she is feeling very anxious. When asked if she is experiencing any pain, she says yes however she has had back pain throughout her pregnancy. She volunteers that she feels dizzy when she stands up and has had a headache for the last few weeks. It has been approximately 15 minutes since the bleeding started.
- What would your initial steps be for the mother? For the baby?
- Name your top two differential diagnoses.
Causes and Risk Factors
The majority of placental abruptions are idiopathic.
Risk factors include:
- maternal hypertension or PIH
- cocaine
- previous abruption (10x risk)
- trauma (MVC, abuse)
- multiparity
- Preterm premature rupture of the membranes (PPROM)
- thrombophilia
- multiple gestation
- polyhydramnios (smaller uterine surface)
- uterine anomaly such as fibroids
- iron deficiency
Intercourse, in and of itself, will not cause abruption.
Pathophysiology
Placental abruption causes bleeding into the decidua basalis layer (the name for the endometrial layer of the uterus during a pregnancy that forms the materal part of the placenta) which causes the placenta to separate. A thin layer of the decidua basalis often remains attached to the placenta after separation. A hematoma can form which then causes further separation and damages the placental tissue. The bleeding can also track into the myometrium causing a couvelaire uterus, which is when the bleeding goes into the peritoneal cavity. This complication causes a significant amount of pain.
Anything that causes rapid decompression of the uterus can be a risk factor for a placental abruption due to shearing forces. Therapeutic amniocentesis for polyhydramnios can occur too fast and cause a separation, same with the birth of the first fetus in a multiple gestation pregnancy. Cocaine use causes blood flow to the placenta to be compromised.
Abruption can cause intrauterine hypoxia due to compromise of the exchange of oxygen at the villi, this is dangerous for the baby. The longer the baby is without oxygen, the greater the chance of hypoxic-ischemic encephalopathy (HIE).
Disseminated intravascular coagulation (DIC) is a condition where excessive clotting and bleeding occurs simultaneously, it can be triggered by an abruption. Both pro-inflammatory and pro-coagulation factors are secreted during an abruption complicated by DIC. DIC is more common when abruption causes fetal demise.
Signs and Symptoms
- history
- physical exam
History
It can be difficult to distinguish a placental abruption from a placenta previa. A placenta previa is when the leading edge of the placenta is within 2cm of the internal os of the cervix on ultrasound. The classical presentation is that a placental abruption is painful bleeding and a placenta previa is painless, however a woman with a placenta previa can also be contracting and thus can be in pain as well. A pelvic exam should not be done until a placenta previa can be ruled out as this can trigger further bleeding.
Placental Abruption |
Placenta Previa |
|
Pain |
Abdominal pain, low back pain |
Painless unless in labour |
Uterus |
Tender, irritable |
Nontender, soft (unless contracting) |
Presentation |
Not associated with abnormal presentation |
Breech or high presenting part |
Fetus |
Fetal heart tracing abnormal, atypical |
Fetal tracing not affected since blood is maternal |
Shock |
Shock/anemia out of proportion to amount of blood seen |
Shock/anemia proportionate to blood seen |
Imaging |
U/S cannot rule out |
U/S sensitive |
Vaginal bleeding or bloody amniotic fluid is present in more than 80% of abruptions, since the majority are external abruptions.
Pain is experienced in >50% of cases. Occasionally an abruption can be painless, it is the blood irritating the uterus that causes the pain so if it is concealed (or walled off by clotting factors) than they may not experience pain.
Physical Exam
Grade |
Uterine Irritability |
Maternal Hemodynamics |
Maternal Fibrinogen |
Fetal Heart Rate |
Mild |
Mild |
Normal |
Normal |
Normal |
Moderate |
Moderate |
Postural hypotension, tachycardic |
Low |
decreased variability, late decelerations |
Severe |
Tetany |
Hypotension, bradycardic |
Very low |
Absent |
In terms of grading the shock, it can be more difficult than in a typical trauma situation. In placental abruption you cannot rely on the amount of blood you see because it can be concealed in the uterus. Because of the hemodynamic changes that occur during pregnancy a pregnant woman can lose a greater amount of blood before clinical signs and symptoms portray the gravity of the situation. A pregnant woman has a greater blood volume thus hypotension may not be as profound as expected particularly if hypertension was present previously. Lastly, vasoconstriction from catecholamines released by the mother can maintain maternal perfusion but leave the placenta compromised, so the fetus can be in more severe distress then the mother.
The contractions that are typical with placental abruption occur very frequently but are of low amplitude; an external monitor may not be sensitive enough to pick up the pattern though.
Investigations
- lab investigations
- diagnostic imaging
Lab Investigations
Maternal Bloodwork: CBC, hematocrit, INR/PTT, fibrinogen, fibrin degradation product (FDP)
Group and screen
Fibrinogen
is converted into fibrin when the clotting cascade is activated. Fibrin
degradation products are produced when a clot has been dissolved by
fibrinolysis, D-dimer being an example of one.
If the mother has DIC, you will see low fibrinogen levels because it has been consumed, and high fibrin degradation product levels. Remember than fibrinogen levels are elevated in a pregnancy so a low-normal level can be significant.
The
Kleihauer-Betke test has limited usefulness for detecting an abruption
however it can be used as a guide for the dose of Rh-immunoglobulin to
administer in Rh negative women. This is a blood test that detects the
amount of fetal hemoglobin in the mothers blood to assess
fetal-maternal hemorrhage.
Diagnostic Imaging
Abruption is usually a clinical diagnosis. Although an ultrasound cannot be relied on to rule out a placental abruption, it can occasionally be seen on one, and it is also useful to assess the fetus. An ultrasound should not be obtained if the mother or fetus is unstable as it will delay treatment.
Differential Diagnosis
- Placenta previa
- Vasa previa
- Uterine rupture (can be confused with a concealed placental abruption)
- Late spontaneous abortion
Treatments
Maternal:
- Large bore IV's with fluids running tailored to the level of shock
- Oxygen for hypotension
- Vital signs monitoring including Foley catheter
- Group and Screen, consider packed red cells, FFP and platelets
- Rhogam if Rh negative
- Bloodwork once stable: CBC, hematocrit, PTT/PT, fibrinogen, fibrin degradation products (FDP)
- A bedside clot test can be done whereby a vial of blood should clot within 6 minutes. Longer may indicate disseminated intravascular coagulation requiring fresh frozen plasma to replace clotting factors
- Oxytocin after delivery to keep the uterus contracted and prevent further hemorrhage
Electronic fetal monitoring
For a mild abruption less than 36wks gestational age, follow and deliver the fetus when it is mature or if condition destabilizes
For a mild abruption greater than 36wks gestational age stabilize the mother and deliver the fetus (vaginally or C/S)
For moderate to severe abruption, deliver the fetus vaginally if no evidence of distress or if fetal demise has already occurred
For moderate to severe abruption, deliver by C/S if there is fetal or maternal distress, labour fails to progress, or breech presentation
Consequences and Course
A significant abruption is very dangerous time for a fetus, with a high mortality rate. A small abruption may not be recognized until the placenta is analyzed after the delivery.
The effect of the abruption on the fetus depends on the severity and the gestational age at which it occurs. An abruption often leads to premature labour and delivery, which has its own set of consequences for the fetus, such as respiratory distress, intraventricular hemorrhage, and necrotizing enterocolitis.
The effect of abruption on the mother depends on the severity. The two main maternal complications are hemorrhagic shock and disseminated intravascular coagulation (DIC), with acute renal failure and cardiac dysfunction being two other important sequelae. DIC is more common when the fetus has died, and often resolves soon after delivery of the fetus. Consider screening for thrombophilias after the delivery, such as factor V leiden, Protein C or S deficiency, lupus anticoagulant, and anticardiolipin antibodies.
Resources and References
Broers T et al. 2004. Occurence of abruptio placentae in Canada: 1990-1997. Chronic Diseases of Canada. 25(2):16-20.
Topic Development
authors: Kim Colangelo, David LaPierre
reviewers:
