
Gastrointestinal Bleeds
last authored:
last reviewed:
Introduction
The Case of...
Causes and Risk Factors
Upper GI bleeds often involve acid. Gastritis and reflux esophagitis are very common causes of more minor bleeds.
Causes of upper GI bleeds include:
|
Causes of lower GI bleeds include:
|
NSAIDs can exacerbate bleeding situations.
DiveticolOSIS is the commonest cause of massive lower GI bleed. Tics are worse in the sigmoid, but can be all over.
The tic's are thin-walled.
Crohn's can rarely cause a large bleed, as the ulcers are so deep. UC rarely bleeds.
if see an abdominal incision/known to have aortic graft, consider aortoenteric fistula. A sentinel bleed often occurs, with minimal bleeding. GET TO THE OR. A true rupture of the aorta will be fatal within minutes.
Angiodysplasia can occur with increasing age.
Mallory-Weiss is characterized
- mucosal tear at the GE junction
- Borhaves (sp)
Duodenal posterior ulcers can bleed if they eat through into the gastro-duodenal artery (anterior ulcers perforate).
Pediatric causes
Acuteinfectious malrotation, volvulus intussusception Meckel's diverticulitis anal fissures Henoch-Schonlein Purpura (HSP) hemolytic uremic syndrome (HUS) coagulopathy |
Chronicanal fissures colitis IBD milk protein allergy polyps (ie hamartoma) coagulopathy
|
Pathophysiology
Signs and Symptoms
- history
- physical exam
History
- liver disease
- medication use (ASA, etc)
Hematemesis - vomiting of blood or coffee ground material.
Melena is black, tarry stool; upper or lower GI bleeds which have been in the system for at least 6 hours.
Hematochezia - passage of maroon or bright red blood with clots by rectum - lower GI bleed or massive upper GI bleed.
Occult GI bleeding is defined as iron deficiency anemia or positive stools for occult blood. No visible blood is seen.
Assess severity by examining hemodynamics and hemoglobin. MCV should be normal - low MCV suggests a chronic component.
If patient is hypotensive or posturally hypotensive, assume there is a massive UPPER GI bleed. Gastroscopy or NG aspiration of bile may be a substitute.
Malfunction of the acid receptors in the duodenum prevents feedback.
Gastric problems with H pylori.
Physical Exam
Hemodynamic status, fever
growth curves in children (FTT)
anal/rectal exam: tags, fissures, fistulas, polyps
Investigations
- lab investigations
- diagnostic imaging
Lab Investigations
Check for liver involvement
Check for problems with coagulopathy: INR, PTT
An elevated BUN can suggest upper GI bleeds, reflecting hemoglobin re-absorption and breakdown.
Diagnostic Imaging
Early endoscopy reduces morbidity, re-bleed rates, and mortality.
Colonoscopy is diagnostic in 72-86% of lower bleeds. If colonoscopy is negative, perform:
Radionuclide imaging can be done using tagged RBCs. It can detect low rates of bleeding 0.1-0.5 ml/min. It can only localize to an area of the abdomen, roughly guiding surgery, and can potentially recommend angiography.
Angiography is very accurate at localizing the source to an anatomic location and can be used to perform embolisation as well. It requires blood loss of 1-1.5 ml/min.
Differential Diagnosis
Treatments
On upper endoscopy, a visible clot or vessel requires admission.
Upper GI bleeds are managed by stabilizing the patient first, assessing the severity of the bleeds, and treating the specific disorder. Ensure two large bore IV's (14 gauge) are in place.
Blood loss can be treated with IV fluids and/or transfusions of packed red cells. Correct any coagulopathy; if INR is >1.5, give fresh frozen plasma.
Consult a gastroenterologist or surgeon, depending on who is available.
Proton pump inhibitors (PPi)s are useful for many causes of upper GI bleeds by facilitating clot stabilization. Use Panteloc 80 mg iv bolus, then 8 mg per hour. PPis are routinely given prior to endoscopy, though evidence lacks.
Octreoide and somatostatin are used to lower portal pressures, reducing splanchnic blood flow and inhibiting gastric acid secretions. They are primarily used in esophageal variceal bleeds; start ASAP is suspected.
Endoscopy is useful for diagnosing cause, stratifying risk of rebleeding using Forrest classification (clean base, flat spots, visible vessels, or active bleeding), and can be used to treat with epinephrine, thermal coagulation, or hemoclips. Clipping near the GE junction collapses the entire column of varices.
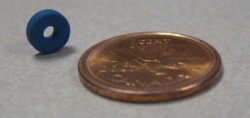 Esophageal varices can also be ligated during endoscopy using bands such as is shown at left
Esophageal varices can also be ligated during endoscopy using bands such as is shown at left
Surgery should get involved if endoscopy is not sufficient, if massive transfusions are required, or if patients remian unstable.
Therapeutic colonoscopy can be done on diverticular bleeds, angiodysplasia.
Esophageal varices will be considered with liver disease or risk factors, but still do endoscopy
- treat with octreotide or somatostatin to reduce portal pressure
- banding
- tamponade with gastric or esophageal balloons
- TIPS: stenting a portal vein tributary into the liver parenchyma
Consequences and Course
With increased bleeding, there is a progression of postural tachycardia, postural hypotension, and hypotension. If either hypotension or postural hypotension (difference of 10-20 mmHg) assume massive bleed.
Resources and References
Topic Development
authors:
reviewers:
