
Glucose Regulation
last authored:
last reviewed:
Introduction
Glucose is the greatly preferred energy source for the brain and the required source for cells with few or no mitochondria, such as RBCs. The body uses various means to ensure blood glucose levels stay high. Glucose can be obtained from three sources: the diet, glycogenolysis, and gluconeogenesis.
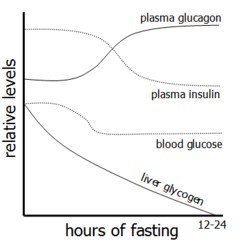
As blood sugar (and insulin) levels fall, the liver begins breaking down glycogen in a process called glycogenolysis to liberate glucose. Muscle glycogen lasts for about an hour of exercise, while liver glycogen stores are longer.
Liver glycogen stores can be used to produce glucose through gluconeogenesis, though stores are sufficient only for a short time (16-24h). Muscle glycogen stores are much higher than that of liver, by muscle lacks glucose-6-phosphatase and therefore cannot contribute to maintenance of blood glucose levels. Instead, it is used as a rapidly mobilizable source of oxidizable glucose for ATP production.
Insulin is an important endocrine signal, lowering blood glucose levels after a meal primarily by increasing muscle and fat uptake and inducing the liver to store it as glycogen.
For extended release of stored gluose, your body goes to your fat stores. FFA and glycerol return to the liver, where they are returned to glucose through gluconeogenesis.
Insulin
Insulin is an important metabolic hormone, regulating blood sugar levels. Recombinant insulin is used to treat diabetes.
It is a two strand polypeptide with 51 amino acids, held together by two disulfide bridges. It is produced as proinsulin and is cleaved to produce insulin, plus C-peptide, an indicator of insulin secretion in early diabetes.
Insulin is the most potent anabolic hormone known, with multiple synthetic and growth-promoting effects. Roughly half of secreted insulin is extracted and used by the liver following its entry into the bloodstream.
Insulin is produced by beta cells in pancreatic Islets of Langerhans, and is stored in cytoplasmic granules before being released. It has a half-life of ~5 minutes; degraded by liver and kidney insulinase. Signals that induce pulsatile insulin expression include:
- blood glucose, the most important signal working through GLUT-2
- amino acids, especially arginine and leucine
- GI hormones such as secretin, glucagon-like peptide 1, and gastric inhibitory peptide
- vagal signaling
- β adrenergic stimulation
Signals that inhibit insulin expression include:
- hypoglycemia
- epinephrine and norepinephrine stimulation of α receptors
Effects on carbohydrate metabolism include:
- increased glucose uptake to muscle and fat by GLUT-4 receptor
- increased liver glycogen synthesis and inhibition of gluconeogenesis and glycogenolysis
- increases muscle glucogen synthesis
- increased glycolysis through transcriptional and translational upregulation of glucokinase, PFK, and pyruvate kinase
Effects on lipid metabolism include:
- decreased adipose TAG degradation by hormone-sensitive lipase
- increased lipoprotein lipase activity, providing FFAs for esterification.
- increased synthesis of FFAs, TAG, and cholesterol
- increased LDL Receptor expression, leading to increased cholesterol uptake
- decreased ketogenesis
Effects on Protein Metabolism include:
- increased amino acid uptake
- increased protein synthesis
- decreased proteolysis
Other Effects include:
- increased ion uptake, especially K+ and PO4-
- stimulates DNA synthesis and cell growth and differentiation in certain cells
Signaling Pathways
Insulin receptor is a cell surface tyrosine kinase; conformational changes following insulin binding leads to autophosphorylation and induction of a signalling cascade. MAP kinase signaling pathway activity leads to cell growth, proliferation, and differentiation, while PI3-K pathway activity leads to GLUT-4 expression and lipid, and protein synthesis.
Insulin binding causes receptor internalization and recycling. In situations of elevated insulin levels, the insulin receptor can be downregulated.
Type I diabetes results from a destruction of beta cells and loss of insulin production
Type II diabetes is caused by systemic insulin resistance
Insulin resistance is characterized by a reduction in ability in insulin's target organs - liver, muscle, and fat - to promote glucose use.
Glucagon
Glucagon is a polypeptide hormone secreted by alpha cells in pancreatic islets of Langerhans. Together with epinephrine, cortisol, and growth hormone, glucagon oppoeses the activity of insulin.
Glucagon binds to its receptor on hepatocytes, activating adenylyl cyclase and the cAMP second messenger system. This results in phosphorylation-mediated changes in key regulatory enzymes.
Glucagon secretion from alpha cells is stimulated by a variety of stimuli:
- low blood glucose is the primary stimulus for glucagon release
- amino acids stimulate both insulin and glucagon release. This prevents insulin-induced hypoglycemia after a protein meal.
- epinephrine from the adrenal medulla, or norepinephrine from the pancreas, stimulate glucagon release in anticipation of increased glucose use during times of stress, trauma, or extreme exercise.
Glucoagon acts primarily on the liver. It causes an immediate rise in glucose levels via breakdown of liver (not muscle) glycogen and an increase in gluconeogenesis. It promotes hepatic oxidation of fatty acids and formation of ketone bodies from acetyl CoA while inhibits cholesterol synthesis by acting on HMG CoA reductase levels. Glucagon increases amino acid uptake by the liver in order top use the carbon skeleton for gluconeogenesis. This decreases plasma amino acid levels.
Incretins
Incretins (GLP-1 and GIP)
pancreas: glucose-dependent insulin secretion and decreased glucagon secretion
- increased beta cell proliferation and decreased apoptosis
muscle and adipose tissue: increased insulin sensitivity, leading to increased glucose uptake and storage
heart: cardioprotection and increased cardiac output
liver: decreased glucose production
brain: increased neuroprotection and decreased appetite
stomach: delay gastic emptying - increased satiety and weight loss
Regulation of Expression
Released from GI tract in respose to...
DPP-IV degrades GLP-1; inhibiting it increases incretin action
